Abstract
Objective
To compare short-term outcomes of Arabs versus Jewish infants in Israel.
Methods
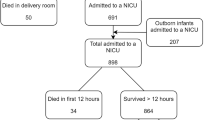
We used the Israel national VLBW infant database to compare adjusted mortality and major morbidities rates of Arabs versus Jewish infants delivered between January 1995 and December 2016. Multivariable logistic regression analyses were performed to study the association of ethnicity with the odds for mortality and neonatal morbidities.
Results
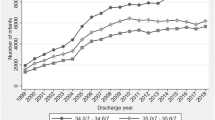
The study population comprised 22431 VLBW, very preterm (<32 weeks gestation) infants (27.7% Arabs and 72.3% Jewish) without congenital malformations. The Arab infants had significantly higher odds ratios for mortality, and most neonatal morbidities. Despite the significant decline in mortality over time in both ethnic groups, the difference in mortality rates remained unchanged over time.
Conclusions
We found significant ethic disparity that remained unchanged over time. Some of the disparities identified in this study may be amenable to improvement through proper policies and education.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Janevic T, Zeitlin J, Auger N, Egorova NN, Herbert P, Balbierz A. et al. Association of race/ethnicity with very preterm neonatal morbidities. JAMA Pediatr. 2018;172:1061–9.
Sigurdson K, Mitchell B, Liu J, Morton C, Gould JB, Lee HC. et al. Racial/ethnic disparities in neonatal intensive care: a systematic review. Pediatrics. 2019;144:e20183114
Boghossian NS, Geraci M, Lorch SA, Phibbs CS, Edwards EM, Horbar JD. Racial and ethnic differences over time in outcomes of infants born less than 30 weeks’ gestation. Pediatrics. 2019;144:e20191106
Dollberg S, Mimouni FB, Lusky A, Reichman B, Israel Neonatal Network. Effect of ethnicity on mortality of very low birthweight infants in Israel. Arch Dis Child Fetal Neonatal Ed. 2003;88:F333–8.
Patel RM, Kandefer S, Walsh MC, Bell EF, Carlo WA, Laptook AR, et al. Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network. Causes and timing of death in extremely premature infants from 2000 through 2011. New Engl J Med. 2015;372:331–40.
Varga P, Berecz B, Gasparics Á, Dombi Z, Varga Z, Jeager J, et al. Morbidity and mortality trends in very-very low birth weight premature infants in light of recent changes in obstetric care. Eur J Obstet Gynecol Reprod Biol. 2017;211:134–9.
Grisaru-Granovsky S, Boyko V, Lerner-Geva L, Hammerman C, Rottenstreich M, Samueloff A, et al. Israel Neonatal Network. The mortality of very low birth weight infants: the benefit and relative impact of changes in population and therapeutic variables. J Matern Fetal Neonatal Med. 2019;32:2443–51.
Israel Society & Culture: Rural Life. Retrieved on 11/01/18 at: http://www.jewishvirtuallibrary.org/rural-life-in-israel
Sher C, Romano-Zelekha O, Green MS, Shohat T. Utilization of prenatal genetic testing by Israeli Moslem women: a national survey. Clin Genet. 2004;65:278–83.
Grisaru-Granovsky S, Reichman B, Lerner-Geva L, Boyko V, Hammerman C, Samueloff A. et al. Mortality and morbidity in preterm small-for gestational-age infants: a population-based study. Am J Obstet Gynecol. 2012;206:150.e1–150.e7.
Grisaru-Granovsky S, Reichman B, Lerner-Geva L, Boyko V, Hammerman C, Samueloff A, Schimmel MS, Israel Neonatal Network. Population-based trends in mortality and neonatal morbidities among singleton, very preterm, very low birth weight infants over 16 years. Early Hum Dev. 2014;90(Dec):821–7.
Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abrahamowicz M. et al. A new and improved population-based Canadian reference for birth weight for gestational age. Pediatrics. 2001;108:E35
Bancalari E, Abdenour GE, Feller R, Gannon J. Bronchopulmonary dysplasia: clinical presentation. J Pediatr. 1979;95:819–23.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L. et al. Neonatal necrotizing enterocolitis: therapeutic decisions based upon clinical staging. Ann Surg. 1978;187:1–7.
Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978;92:529–34.
The Committee for the Classification of Retinopathy of Prematurity. An international classification of retinopathy of prematurity. Arch Ophthalmol. 1984;102:1130–4.
Hollowell J, Oakley L, Kurinczuk JJ, Brocklehurst P, Gray R. The effectiveness of antenatal care programmes to reduce infant mortality and preterm birth in socially disadvantaged and vulnerable women in high-income countries: a systematic review. BMC Pregnancy Childbirth. 2011;11;13.
Corchia C, Ferrante P, Da Frè M, Di Lallo D, Gagliardi L, Carnielli V, et al. Cause-specific mortality of very preterm infants and antenatal events. J Pediatr. 2013;162:1125–32.
Zhang H, Liu J, Liu T, Wang Y, Dai W. Antenatal maternal medication administration in preventing respiratory distress syndrome of premature infants: a network meta-analysis. Clin Respir J. 2018;12:2480–90.
Boghossian NS, Geraci M, Edwards EM, Horbar JD. Sex differences in mortality and morbidity of infants born at less than 30 weeks’ gestation. Pediatrics. 2018;142:e20182352. pii
Nayeri F, Dalili H, Nili F, Amini E, Ardehali A, Khoshkrood Mansoori B, et al. Risk factors for neonatal mortality among very low birth weight neonates. Acta Med Iran. 2013;51:297–302.
Steurer MA, Nawaytou H, Guslits E, Colglazier E, Teitel D, Fineman JR, et al. Mortality in infants with bronchopulmonary dysplasia: data from cardiac catheterization. Pediatr Pulmonol. 2019;54:804–13.
Schindler T, Koller-Smith L, Lui K, Bajuk B, Bolisetty S, New South Wales and Australian Capital Territory Neonatal Intensive Care Units’ Data Collection. Causes of death in very preterm infants cared for in neonatal intensive care units: a population-based retrospective cohort study. BMC Pediatr. 2017;17:59.
Halon E. Jewish, Arab women marrying later than a decade ago, the Jeruslaem post March 6. 2019. https://www.jpost.com/Israel-News/Jewish-Arab-women-marrying-later-than-decade-ago-582611. Retrieved on 16 June 2019.
Fuchs H. Education and employment among young Israeli arabs. http://taubcenter.org.il/wp-content/files_mf/arabisraelisinhighereducation.pdf. Retrieved on 16 June 2019.
Sauer MV. Reproduction at an advanced maternal age and maternal health. Fertil Steril. 2015;103:1136–43.
Ben Natan M, Ashkenazi M, Masarwe S. Intentions of Muslim Arab women in Israel to attend prenatal classes. Women Birth. 2016;29:e8–12.
Slidsborg C, Jensen A, Forman JL, Rasmussen S, Bangsgaard R, Fledelius HC, et al. Neonatal risk factors for treatment-demanding retinopathy of prematurity: A Danish National Study. Ophthalmology. 2016;123:796–803.
Yu C, Yi J, Yin X, Deng Y, Liao Y, Li X. Correlation of interactions between NOS3 polymorphisms and oxygen therapy with retinopathy of prematurity susceptibility. Int J Clin Exp Pathol. 2015;8:15250–4.
Dhaliwal CA, Fleck BW, Wright E, Graham C, McIntosh N. Retinopathy of prematurity in small-for-gestational age infants compared with those of appropriate size for gestational age. Arch Dis Child Fetal Neonatal Ed. 2009;94:F193–5.
Husain SM, Sinha AK, Bunce C, Arora P, Lopez W, Mun KS, et al. Relationships between maternal ethnicity, gestational age, birth weight, weight gain, and severe retinopathy of prematurity. J Pediatr. 2013;163:67–72.
Holmström G, van Wijngaarden P, Coster DJ, Williams KA. Genetic susceptibility to retinopathy of prematurity: the evidence from clinical and experimental animal studies. Br J Ophthalmol. 2007;91:1704–8.
Kasirer MY, Mimouni FB, Bin-Nun A, Schimmel MS. Opinions of Israeli neonatologists about life and death decisions in neonates. J Perinatol. 2018;38:1101–5.
Schimmel MS, Mimouni FB, Steinberg A, Kasirer MY. Ethical dilemmas in neonatology - four theoretical cases and three monotheistic approaches: a pilot study. Isr Med Assoc J. 2019;5:314–7.
Morales LS, Staiger D, Horbar JD, Carpenter J, Kenny M, Geppert J, et al. Mortality among very low-birthweight infants in hospitals serving minority populations. Am J Public Health. 2005;95:2206–12.
Lake ET, Staiger D, Edwards EM, Smith JG, Rogowski JA. Nursing care disparities in neonatal intensive care units. Health Serv Res. 2018;53:3007–26. Aug
Funding
The Israel National very low birth weight infant database is supported partially by the Israel Center for Disease Control and the Ministry of Health.
Author information
Authors and Affiliations
Consortia
Contributions
Y.K.: contributed substantially to the conception and design of the study, interpretation of the data, drafted the initial manuscript, and approved the final manuscript as submitted. B.R.: contributed substantially to the conception and design of the study, analysis, and interpretation of the data, drafting the article, and has approved the final version of the article. I.Z.-P.: contributed substantially to the design of the study, analysis and interpretation of the data, revision of the article for important intellectual content and has approved the final version of the article. A.B.N. contributed substantially to the design of the study, analysis and interpretation of the data, revision of the article for important intellectual content and has approved the final version of the article. L.L.-G.: contributed substantially to the data acquisition, interpretation of the data, and revision of the article for important intellectual content and has approved the final version of the article. F.B.M.: contributed substantially to the conception and design of the study, analysis, and interpretation of the data, drafting the article, and has approved the final version of the article.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kasirer, Y., Reichman, B., Zaslavsky-Paltiel, I. et al. Short-term outcomes of Jewish and Arab preterms: a population-based comparison. J Perinatol 41, 453–459 (2021). https://doi.org/10.1038/s41372-020-0743-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0743-9