Abstract
Although often considered a single-entity, chronic kidney disease (CKD) comprises many pathophysiologically distinct disorders that result in persistently abnormal kidney structure and/or function, and encompass both monogenic and polygenic aetiologies. Rare inherited forms of CKD frequently span diverse phenotypes, reflecting genetic phenomena including pleiotropy, incomplete penetrance and variable expressivity. Use of chromosomal microarray and massively parallel sequencing technologies has revealed that genomic disorders and monogenic aetiologies contribute meaningfully to seemingly complex forms of CKD across different clinically defined subgroups and are characterized by high genetic and phenotypic heterogeneity. Investigations of prevalent genomic disorders in CKD have integrated genetic, bioinformatic and functional studies to pinpoint the genetic drivers underlying their renal and extra-renal manifestations, revealing both monogenic and polygenic mechanisms. Similarly, massively parallel sequencing-based analyses have identified gene- and allele-level variation that contribute to the clinically diverse phenotypes observed for many monogenic forms of nephropathy. Genome-wide sequencing studies suggest that dual genetic diagnoses are found in at least 5% of patients in whom a genetic cause of disease is identified, highlighting the fact that complex phenotypes can also arise from multilocus variation. A multifaceted approach that incorporates genetic and phenotypic data from large, diverse cohorts will help to elucidate the complex relationships between genotype and phenotype for different forms of CKD, supporting personalized medicine for individuals with kidney disease.
Key points
-
Chronic kidney disease (CKD) is a complex disorder comprising many rarer, pathophysiologically distinct conditions that encompass both monogenic and polygenic forms, which share the common feature of leading to persistent anomalies in renal structure and/or function.
-
Rare hereditary causes of CKD often show high phenotypic heterogeneity, which can result from pleiotropy, incomplete penetrance or variable expressivity.
-
Microarray and massively parallel sequencing studies have shown that both genomic disorders and monogenic diseases account for a meaningful proportion of cases across different clinical subtypes of CKD.
-
Copy number variants at the 17q12, 22q11.2 and 16p11.2 loci are recurrent genomic disorders among patients with CKD and display diverse and highly variable multiorgan manifestations, which can reflect gene dosage sensitivity and epistatic and epigenetic effects.
-
Although classically considered to be clinically homogeneous, common monogenic causes of CKD, such as autosomal-dominant polycystic kidney disease, type IV collagen-associated nephropathy and autosomal-dominant tubulointerstitial kidney disease, display variable penetrance and expressivity, in part due to gene- and allele-level variation.
-
Multilocus variation, involving variants for multiple genetic conditions, can confer complex phenotypes and has been detected in at least 5% of positive cases from genome-wide testing.
-
Novel techniques that integrate genetic sequencing, experimental assays and clinical data, such as reverse phenotyping, functional screening of potentially pathogenic variants, and genetic and phenotypic risk scores, will support greater understanding of the phenotypic complexity of different forms of CKD.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Webster, A. C., Nagler, E. V., Morton, R. L. & Masson, P. Chronic kidney disease. Lancet 389, 1238–1252 (2017).
Devuyst, O. et al. Rare inherited kidney diseases: challenges, opportunities, and perspectives. Lancet 383, 1844–1859 (2014).
Skrunes, R., Svarstad, E., Reisaeter, A. V. & Vikse, B. E. Familial clustering of ESRD in the Norwegian population. Clin. J. Am. Soc. Nephrol. 9, 1692–1700 (2014).
Connaughton, D. M. et al. The Irish kidney gene project–prevalence of family history in patients with kidney disease in ireland. Nephron 130, 293–301 (2015).
McClellan, W. M. et al. Individuals with a family history of ESRD are a high-risk population for CKD: implications for targeted surveillance and intervention activities. Am. J. Kidney Dis. 53, S100–S106 (2009).
Fox, C. S. et al. Genomewide linkage analysis to serum creatinine, GFR, and creatinine clearance in a community-based population: the Framingham Heart Study. J. Am. Soc. Nephrol. 15, 2457–2461 (2004).
Arpegard, J. et al. Comparison of heritability of Cystatin C- and creatinine-based estimates of kidney function and their relation to heritability of cardiovascular disease. J. Am. Heart Assoc. 4, e001467 (2015).
Gorski, M. et al. 1000 genomes-based meta-analysis identifies 10 novel loci for kidney function. Sci. Rep. 7, 45040 (2017).
Moulin, F. et al. A population-based approach to assess the heritability and distribution of renal handling of electrolytes. Kidney Int. 92, 1536–1543 (2017).
Lieske, J. C., Turner, S. T., Edeh, S. N., Smith, J. A. & Kardia, S. L. Heritability of urinary traits that contribute to nephrolithiasis. Clin. J. Am. Soc. Nephrol. 9, 943–950 (2014).
Zanetti, D. et al. Identification of 22 novel loci associated with urinary biomarkers of albumin, sodium, and potassium excretion. Kidney Int. 95, 1197–1208 (2019).
Leu, C. et al. Polygenic burden in focal and generalized epilepsies. Brain 142, 3473–3481 (2019).
Speed, D. et al. Describing the genetic architecture of epilepsy through heritability analysis. Brain 137, 2680–2689 (2014).
El-Fishawy, P. & State, M. W. The genetics of autism: key issues, recent findings, and clinical implications. Psychiatr. Clin. North. Am. 33, 83–105 (2010).
Vorstman, J. A. S. et al. Autism genetics: opportunities and challenges for clinical translation. Nat. Rev. Genet. 18, 362–376 (2017).
Khera, A. V. et al. Genome-wide polygenic scores for common diseases identify individuals with risk equivalent to monogenic mutations. Nat. Genet. 50, 1219–1224 (2018). This study created and validated genome-wide polygenic risk scores for multiple common conditions, including coronary artery disease, type 2 diabetes and breast cancer, and demonstrated that individuals at the uppermost risk percentiles had disease risk equivalent to those with pathogenic mutations for rare monogenic forms of these conditions.
Khera, A. V. et al. Whole-genome sequencing to characterize monogenic and polygenic contributions in patients hospitalized with early-onset myocardial infarction. Circulation 139, 1593–1602 (2019).
Katsanis, N. The continuum of causality in human genetic disorders. Genome Biol. 17, 233 (2016).
Lupski, J. R., Belmont, J. W., Boerwinkle, E. & Gibbs, R. A. Clan genomics and the complex architecture of human disease. Cell 147, 32–43 (2011).
Genovese, G. et al. Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science 329, 841–845 (2010).
Tzur, S. et al. Missense mutations in the APOL1 gene are highly associated with end stage kidney disease risk previously attributed to the MYH9 gene. Hum. Genet. 128, 345–350 (2010). Together with Genovese et al., this investigation demonstrated that two common missense variants in the apoliproprotein L1 gene significantly increased the risk of a variety of forms of non-diabetic CKD among individuals of sub-Saharan African descent, and point to a potential mechanism for their being positively selected for over the course of human evolution.
Stanescu, H. C. et al. Risk HLA-DQA1 and PLA(2)R1 alleles in idiopathic membranous nephropathy. N. Engl. J. Med. 364, 616–626 (2011). This genome-wide association study found that homozygotes for risk alleles at the HLA-DQA1 and PLA2R1 loci had nearly an 80-fold higher odds of developing idopathic membranous nephropathy than those without these alleles. These findings highlight that common variants can result in a genetic architecture similar to that of digenic inheritance arising from rare mutations at two different loci.
Xie, J. et al. The genetic architecture of membranous nephropathy and its potential to improve non-invasive diagnosis. Nat. Commun. 11, 1600 (2020). This investigation identified two additional risk alleles for idiopathic membranous nephropathy and examines the ancestry-specific effects of variation at the HLA locus. Using the genome-wide significant risk loci detected, they create a genetic risk score that can correctly reclassify up to 37% of affected individuals with negative results on serological screening, emphasizing the potential of genetic risk score to empower non-invasive diagnosis of kidney disease.
Connaughton, D. M. & Hildebrandt, F. Personalized medicine in chronic kidney disease by detection of monogenic mutations. Nephrol. Dial. Transplant 35, 390–397 (2020).
Groopman, E. E., Rasouly, H. M. & Gharavi, A. G. Genomic medicine for kidney disease. Nat. Rev. Nephrol. 14, 83–104 (2018).
Eknoyan, G. et al. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int. Suppl. 3, 19–62 (2013).
Graham, S. E. et al. Sex-specific and pleiotropic effects underlying kidney function identified from GWAS meta-analysis. Nat. Commun. 10, 1847 (2019).
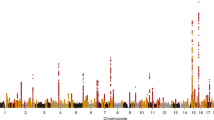
Wuttke, M. et al. A catalog of genetic loci associated with kidney function from analyses of a million individuals. Nat. Genet. 51, 957–972 (2019). This genome-wide association study of a combined cohort of over one million individuals identified 166 novel kidney function-associated loci and utilized gene expression data to prioritize candidate genes for future study.
Mitchell, K. J. What is complex about complex disorders? Genome Biol. 13, 237 (2012).
Braun, D. A. et al. Whole exome sequencing identifies causative mutations in the majority of consanguineous or familial cases with childhood-onset increased renal echogenicity. Kidney Int. 89, 468–475 (2016).
Gee, H. Y. et al. Whole-exome resequencing distinguishes cystic kidney diseases from phenocopies in renal ciliopathies. Kidney Int. 85, 880–887 (2014).
Bierzynska, A. et al. Genomic and clinical profiling of a national nephrotic syndrome cohort advocates a precision medicine approach to disease management. Kidney Int. 91, 937–947 (2017). This investigation integrated exome sequencing and detailed phenotyping to identify monogenic forms of early-onset steroid-resistant nephrotic syndrome and develop an evidence-based framework for the diagnosis and management of this clinically and aetiologically heterogeneous disorder.
Landini, S. et al. Reverse phenotyping after whole-exome sequencing in steroid-resistant nephrotic syndrome. Clin. J. Am. Soc. Nephrol. 15, 89–100 (2020).
Vivante, A. et al. Exome sequencing discerns syndromes in patients from consanguineous families with congenital anomalies of the kidneys and urinary tract. J. Am. Soc. Nephrol. 28, 69–75 (2017). This study applied exome sequencing and reverse phenotyping to differentiate individuals with monogenic forms of congenital anomalies of the kidney and urinary tract from those with mutations in phenocopy genes, pointing to the diagnostic value of genome-wide sequencing among this patient population.
Schimmenti, L. A. Renal coloboma syndrome. Eur. J. Hum. Genet. 19, 1207–1212 (2011).
Eccles, M. R. & Schimmenti, L. A. Renal-coloboma syndrome: a multi-system developmental disorder caused by PAX2 mutations. Clin. Genet. 56, 1–9 (1999).
Vivante, A. et al. Dominant PAX2 mutations may cause steroid-resistant nephrotic syndrome and FSGS in children. Pediatr. Nephrol. 34, 1607–1613 (2019).
Barua, M. et al. Mutations in PAX2 associate with adult-onset FSGS. J. Am. Soc. Nephrol. 25, 1942–1953 (2014).
Bower, M. et al. Update of PAX2 mutations in renal coloboma syndrome and establishment of a locus-specific database. Hum. Mutat. 33, 457–466 (2012).
Adam, J. et al. A wide spectrum of phenotypes in a family with renal coloboma syndrome caused by a mutation. Clin. Kidney J. 6, 410–413 (2013).
Riordan, J. D. & Nadeau, J. H. From peas to disease: modifier genes, network resilience, and the genetics of health. Am. J. Hum. Genet. 101, 177–191 (2017).
Lettre, G. et al. DNA polymorphisms at the BCL11A, HBS1L-MYB, and beta-globin loci associate with fetal hemoglobin levels and pain crises in sickle cell disease. Proc. Natl Acad. Sci. USA 105, 11869–11874 (2008).
Louie, C. M. et al. AHI1 is required for photoreceptor outer segment development and is a modifier for retinal degeneration in nephronophthisis. Nat. Genet. 42, 175–180 (2010).
Nozu, K. et al. Molecular analysis of digenic inheritance in Bartter syndrome with sensorineural deafness. J. Med. Genet. 45, 182–186 (2008).
Schlingmann, K. P. et al. Salt wasting and deafness resulting from mutations in two chloride channels. N. Engl. J. Med. 350, 1314–1319 (2004).
Devuyst, O., Olinger, E. & Rampoldi, L. Uromodulin: from physiology to rare and complex kidney disorders. Nat. Rev. Nephrol. 13, 525–544 (2017).
Lopez-Rivera, E. et al. Genetic drivers of kidney defects in the DiGeorge syndrome. N. Engl. J. Med. 376, 742–754 (2017).
Verbitsky, M. et al. Genomic imbalances in pediatric patients with chronic kidney disease. J. Clin. Invest. 125, 2171–2178 (2015). This study demonstrates that genomic disorders can be found across paediatric patients clinically diagnosed with a variety of forms of CKD, supporting that genomic disorders contribute broadly to early-onset CKD.
Verbitsky, M. et al. The copy number variation landscape of congenital anomalies of the kidney and urinary tract. Nat. Genet. 51, 117–127 (2019).
Caruana, G. et al. Copy-number variation associated with congenital anomalies of the kidney and urinary tract. Pediatr. Nephrol. 30, 487–495 (2015).
Faure, A. et al. DNA copy number variants: a potentially useful predictor of early onset renal failure in boys with posterior urethral valves. J. Pediatr. Urol. 12, 227.E1–227.E7 (2016).
Sanna-Cherchi, S. et al. Copy-number disorders are a common cause of congenital kidney malformations. Am. J. Hum. Genet. 91, 987–997 (2012). This analysis of chromosomal microarray data from nearly 500 patients with renal hypodysplasia found that 16.6% of them harboured diagnostic copy number variants. Importantly, the majority of known genomic disorders identified were associated with developmental delay or neuropsychiatric disease, pointing to the utility of chromosomal microarray among individuals with congenital anomalies of the kidney and urinary tract for early detection and targeted management in individuals with such syndromic forms of disease.
Sanna-Cherchi, S., Westland, R., Ghiggeri, G. M. & Gharavi, A. G. Genetic basis of human congenital anomalies of the kidney and urinary tract. J. Clin. Invest. 128, 4–15 (2018).
Nicolaou, N., Renkema, K. Y., Bongers, E. M., Giles, R. H. & Knoers, N. V. Genetic, environmental, and epigenetic factors involved in CAKUT. Nat. Rev. Nephrol. 11, 720–731 (2015).
Crawford, K. et al. Medical consequences of pathogenic CNVs in adults: analysis of the UK Biobank. J. Med. Genet. 56, 131–138 (2019).
Van Batavia, J. P. et al. Anomalies of the genitourinary tract in children with 22q11.2 deletion syndrome. Am. J. Med. Genet. A 179, 381–385 (2019).
Jacquemont, S. et al. Mirror extreme BMI phenotypes associated with gene dosage at the chromosome 16p11.2 locus. Nature 478, 97–102 (2011).
Bellanne-Chantelot, C. et al. Large genomic rearrangements in the hepatocyte nuclear factor-1beta (TCF2) gene are the most frequent cause of maturity-onset diabetes of the young type 5. Diabetes 54, 3126–3132 (2005).
Mefford, H. C. et al. Recurrent reciprocal genomic rearrangements of 17q12 are associated with renal disease, diabetes, and epilepsy. Am. J. Hum. Genet. 81, 1057–1069 (2007).
Moreno-De-Luca, D. et al. Deletion 17q12 is a recurrent copy number variant that confers high risk of autism and schizophrenia. Am. J. Hum. Genet. 87, 618–630 (2010).
Nagamani, S. C. et al. Clinical spectrum associated with recurrent genomic rearrangements in chromosome 17q12. Eur. J. Hum. Genet. 18, 278–284 (2010).
Mitchel, M. W. et al. 17q12 recurrent deletion syndrome. GeneReviews https://www.ncbi.nlm.nih.gov/books/NBK401562/ (8 Dec 2016).
Mefford, H., Mitchell, E. & Hodge, J. 17q12 recurrent duplication. GeneReviews https://www.ncbi.nlm.nih.gov/books/NBK344340/ (25 Feb 2016).
Clissold, R. L., Hamilton, A. J., Hattersley, A. T., Ellard, S. & Bingham, C. HNF1B-associated renal and extra-renal disease-an expanding clinical spectrum. Nat. Rev. Nephrol. 11, 102–112 (2015).
El-Khairi, R. & Vallier, L. The role of hepatocyte nuclear factor 1beta in disease and development. Diabetes Obes. Metab. 18, 23–32 (2016).
Bingham, C. et al. Mutations in the hepatocyte nuclear factor-1beta gene are associated with familial hypoplastic glomerulocystic kidney disease. Am. J. Hum. Genet. 68, 219–224 (2001).
Horikawa, Y. et al. Mutation in hepatocyte nuclear factor-1 beta gene (TCF2) associated with MODY. Nat. Genet. 17, 384–385 (1997).
Choe, S. K., Hirsch, N., Zhang, X. & Sagerstrom, C. G. hnf1b genes in zebrafish hindbrain development. Zebrafish 5, 179–187 (2008).
Makki, N. & Capecchi, M. R. Identification of novel Hoxa1 downstream targets regulating hindbrain, neural crest and inner ear development. Dev. Biol. 357, 295–304 (2011).
Clissold, R. L. et al. Chromosome 17q12 microdeletions but not intragenic HNF1B mutations link developmental kidney disease and psychiatric disorder. Kidney Int. 90, 203–211 (2016).
Bedont, J. L. et al. Lhx1 controls terminal differentiation and circadian function of the suprachiasmatic nucleus. Cell Rep. 7, 609–622 (2014).
Zhao, Y. et al. LIM-homeodomain proteins Lhx1 and Lhx5, and their cofactor Ldb1, control Purkinje cell differentiation in the developing cerebellum. Proc. Natl Acad. Sci. USA 104, 13182–13186 (2007).
Girirajan, S. et al. Refinement and discovery of new hotspots of copy-number variation associated with autism spectrum disorder. Am. J. Hum. Genet. 92, 221–237 (2013).
Laffargue, F. et al. Towards a new point of view on the phenotype of patients with a 17q12 microdeletion syndrome. Arch. Dis. Child. 100, 259–264 (2015).
Clissold, R. L. et al. Genome-wide methylomic analysis in individuals with HNF1B intragenic mutation and 17q12 microdeletion. Clin. Epigenetics 10, 97 (2018).
van Amen-Hellebrekers, C. J. et al. Duplications of SLC1A3: associated with ADHD and autism. Eur. J. Med. Genet. 59, 373–376 (2016).
Weiss, L. A. et al. Association between microdeletion and microduplication at 16p11.2 and autism. N. Engl. J. Med. 358, 667–675 (2008).
Kaminsky, E. B. et al. An evidence-based approach to establish the functional and clinical significance of copy number variants in intellectual and developmental disabilities. Genet. Med. 13, 777–784 (2011).
Bochukova, E. G. et al. Large, rare chromosomal deletions associated with severe early-onset obesity. Nature 463, 666–670 (2010).
Zufferey, F. et al. A 600kb deletion syndrome at 16p11.2 leads to energy imbalance and neuropsychiatric disorders. J. Med. Genet. 49, 660–668 (2012).
Miller, D. T. et al. 16p11.2 recurrent microdeletion. GeneReviews https://www.ncbi.nlm.nih.gov/books/NBK11167 (updated 10 Dec 2015).
Steinman, K. J. et al. 16p11.2 deletion and duplication: characterizing neurologic phenotypes in a large clinically ascertained cohort. Am. J. Med. Genet. A 170, 2943–2955 (2016).
Chapman, D. L., Agulnik, I., Hancock, S., Silver, L. M. & Papaioannou, V. E. Tbx6, a mouse T-Box gene implicated in paraxial mesoderm formation at gastrulation. Dev. Biol. 180, 534–542 (1996).
Chapman, D. L. & Papaioannou, V. E. Three neural tubes in mouse embryos with mutations in the T-box gene Tbx6. Nature 391, 695–697 (1998).
Concepcion, D. et al. Cell lineage of timed cohorts of Tbx6-expressing cells in wild-type and Tbx6 mutant embryos. Biol. Open. 6, 1065–1073 (2017).
Wu, N. et al. TBX6 null variants and a common hypomorphic allele in congenital scoliosis. N. Engl. J. Med. 372, 341–350 (2015).
MacEwen, G. D., Winter, R. B. & Hardy, J. H. Evaluation of kidney anomalies in congenital scoliosis. J. Bone Jt. Surg. Am. 54, 1451–1454 (1972).
Yang, N. et al. Human and mouse studies establish TBX6 in Mendelian CAKUT and as a potential driver of kidney defects associated with the 16p11.2 microdeletion syndrome. Kidney Int. (2020).
Dong, S. et al. Noncoding rare variants of TBX6 in congenital anomalies of the kidney and urinary tract. Mol. Genet. Genomics 294, 493–500 (2019).
McDonald-McGinn, D. M. et al. 22q11.2 deletion syndrome. GeneReviews https://www.ncbi.nlm.nih.gov/books/NBK1523/ (updated 27 Feb 2020).
Morrow, B. E., McDonald-McGinn, D. M., Emanuel, B. S., Vermeesch, J. R. & Scambler, P. J. Molecular genetics of 22q11.2 deletion syndrome. Am. J. Med. Genet. A 176, 2070–2081 (2018).
Shaikh, T. H. et al. Chromosome 22-specific low copy repeats and the 22q11.2 deletion syndrome: genomic organization and deletion endpoint analysis. Hum. Mol. Genet. 9, 489–501 (2000).
Merscher, S. et al. TBX1 is responsible for cardiovascular defects in velo-cardio-facial/DiGeorge syndrome. Cell 104, 619–629 (2001).
Yagi, H. et al. Role of TBX1 in human del22q11.2 syndrome. Lancet 362, 1366–1373 (2003).
Paylor, R. et al. Tbx1 haploinsufficiency is linked to behavioral disorders in mice and humans: implications for 22q11 deletion syndrome. Proc. Natl Acad. Sci. USA 103, 7729–7734 (2006).
Haller, M., Mo, Q., Imamoto, A. & Lamb, D. J. Murine model indicates 22q11.2 signaling adaptor CRKL is a dosage-sensitive regulator of genitourinary development. Proc. Natl Acad. Sci. USA 114, 4981–4986 (2017).
Guris, D. L., Fantes, J., Tara, D., Druker, B. J. & Imamoto, A. Mice lacking the homologue of the human 22q11.2 gene CRKL phenocopy neurocristopathies of DiGeorge syndrome. Nat. Genet. 27, 293–298 (2001).
Racedo, S. E. et al. Mouse and human CRKL is dosage sensitive for cardiac outflow tract formation. Am. J. Hum. Genet. 96, 235–244 (2015).
Hays, T., Groopman, E. E. & Gharavi, A. G. Genetic testing for kidney disease of unknown etiology. Kidney Int. https://doi.org/10.1016/j.kint.2020.03.031 (2020).
Groopman, E. E. et al. Diagnostic utility of exome sequencing for kidney disease. N. Engl. J. Med. 380, 142–151 (2019). This study found that exome sequencing in a combined cohort of 3,315 individuals with CKD of diverse causes identified a monogenic cause in nearly 1 in 10 cases, highlighting the diagnostic utility of genome-wide sequencing for patients with kidney disease.
Lata, S. et al. Whole-exome sequencing in adults with chronic kidney disease: a pilot study. Ann. Intern. Med. 168, 100–109 (2018).
Mallett, A. J. et al. Massively parallel sequencing and targeted exomes in familial kidney disease can diagnose underlying genetic disorders. Kidney Int. 92, 1493–1506 (2017). This investigation applied targeted massively parallel sequencing and phenotype-driven analysis led by a multidisciplinary team to identify a monogenic cause in over 40% of individuals referred for evaluation of familial kidney disease. The high detection rate supports the efficacy of this approach for the work-up of patients suspected to have an inherited form of CKD.
Connaughton, D. M. et al. Monogenic causes of chronic kidney disease in adults. Kidney Int. 95, 914–928 (2019).
Mansilla, M. A. et al. Targeted broad-based genetic testing by next-generation sequencing informs diagnosis and facilitates management in patients with kidney diseases. Nephrol. Dial. Transplant. https://doi.org/10.1093/ndt/gfz173 (2019).
Rao, J. et al. Genetic spectrum of renal disease for 1001 Chinese children based on a multicenter registration system. Clin. Genet. 96, 402–410 (2019).
Malone, A. F. et al. Rare hereditary COL4A3/COL4A4 variants may be mistaken for familial focal segmental glomerulosclerosis. Kidney Int. 86, 1253–1259 (2014).
Kashtan, C. E. et al. Alport syndrome: a unified classification of genetic disorders of collagen IV alpha345: a position paper of the Alport Syndrome Classification Working Group. Kidney Int. 93, 1045–1051 (2018).
Savige, J. et al. Expert consensus guidelines for the genetic diagnosis of Alport syndrome. Pediatr. Nephrol. 34, 1175–1189 (2019).
Gast, C. et al. Collagen (COL4A) mutations are the most frequent mutations underlying adult focal segmental glomerulosclerosis. Nephrol. Dial. Transpl. 31, 961–970 (2016).
Yao, T. et al. Integration of genetic testing and pathology for the diagnosis of adults with FSGS. Clin. J. Am. Soc. Nephrol. 14, 213–223 (2019).
Gulati, A. et al. Collagen IV gene mutations in adults with bilateral renal cysts and CKD. Kidney Int. Rep. 5, 103–108 (2020).
Wuttke, M. et al. A COL4A5 mutation with glomerular disease and signs of chronic thrombotic microangiopathy. Clin. Kidney J. 8, 690–694 (2015).
Salem, R. M. et al. Genome-wide association study of diabetic kidney disease highlights biology involved in glomerular basement membrane collagen. J. Am. Soc. Nephrol. 30, 2000–2016 (2019).
Huang, K. L. et al. Pathogenic germline variants in 10,389 adult cancers. Cell 173, 355–370 e314 (2018).
Zhang, J. et al. Germline mutations in predisposition genes in pediatric cancer. N. Engl. J. Med. 373, 2336–2346 (2015).
Fiorentino, M. et al. Renal biopsy in patients with diabetes: a pooled meta-analysis of 48 studies. Nephrol. Dial. Transpl. 32, 97–110 (2017).
Sharma, S. G. et al. The modern spectrum of renal biopsy findings in patients with diabetes. Clin. J. Am. Soc. Nephrol. 8, 1718–1724 (2013).
Fogo, A. et al. Accuracy of the diagnosis of hypertensive nephrosclerosis in African Americans: a report from the African American study of kidney disease (AASK) trial. AASK Pilot Study Investigators. Kidney Int. 51, 244–252 (1997).
Freedman, B. I., Iskander, S. S., Buckalew, V. M. Jr, Burkart, J. M. & Appel, R. G. Renal biopsy findings in presumed hypertensive nephrosclerosis. Am. J. Nephrol. 14, 90–94 (1994).
Marcantoni, C., Ma, L. J., Federspiel, C. & Fogo, A. B. Hypertensive nephrosclerosis in African Americans versus caucasians. Kidney Int. 62, 172–180 (2002).
Liu, C. et al. Meta-analysis identifies common and rare variants influencing blood pressure and overlapping with metabolic trait loci. Nat. Genet. 48, 1162–1170 (2016).
Warren, H. R. et al. Genome-wide association analysis identifies novel blood pressure loci and offers biological insights into cardiovascular risk. Nat. Genet. 49, 403–415 (2017).
Sandholm, N. et al. The genetic landscape of renal complications in type 1 diabetes. J. Am. Soc. Nephrol. 28, 557–574 (2017).
van Zuydam, N. R. et al. A genome-wide association study of diabetic kidney disease in subjects with type 2 diabetes. Diabetes 67, 1414–1427 (2018).
De Tomasi, L. et al. Mutations in GREB1L cause bilateral kidney agenesis in humans and mice. Am. J. Hum. Genet. 101, 803–814 (2017).
Sanna-Cherchi, S. et al. Exome-wide association study identifies GREB1L mutations in congenital kidney malformations. Am. J. Hum. Genet. 101, 789–802 (2017).
Kingsmore, S. F. et al. A randomized, controlled trial of the analytic and diagnostic performance of singleton and trio, rapid genome and exome sequencing in ill infants. Am. J. Hum. Genet. 105, 719–733 (2019).
Goodwin, S., McPherson, J. D. & McCombie, W. R. Coming of age: ten years of next-generation sequencing technologies. Nat. Rev. Genet. 17, 333–351 (2016).
Cummings, B. B. et al. Improving genetic diagnosis in Mendelian disease with transcriptome sequencing. Sci. Transl. Med. 9, eaal5209 (2017).
King, D. A. et al. Detection of structural mosaicism from targeted and whole-genome sequencing data. Genome Res. 27, 1704–1714 (2017).
Wright, C. F. et al. Clinically-relevant postzygotic mosaicism in parents and children with developmental disorders in trio exome sequencing data. Nat. Commun. 10, 2985 (2019).
Gardner, E. J. et al. Contribution of retrotransposition to developmental disorders. Nat. Commun. 10, 4630 (2019).
Ju, Y. S. et al. Somatic mutations reveal asymmetric cellular dynamics in the early human embryo. Nature 543, 714–718 (2017).
Lionel, A. C. et al. Improved diagnostic yield compared with targeted gene sequencing panels suggests a role for whole-genome sequencing as a first-tier genetic test. Genet. Med. 20, 435–443 (2018).
Redin, C. et al. The genomic landscape of balanced cytogenetic abnormalities associated with human congenital anomalies. Nat. Genet. 49, 36–45 (2017).
Vabres, P. et al. Postzygotic inactivating mutations of RHOA cause a mosaic neuroectodermal syndrome. Nat. Genet. 51, 1438–1441 (2019).
Mohammadi, P. et al. Genetic regulatory variation in populations informs transcriptome analysis in rare disease. Science 366, 351–356 (2019). This study incorporated tissue-specific and population-level RNA sequencing data to identify causal genes among patients with genetically unresolved disease, demonstrating the utility of transcriptomics for the diagnosis of rare disease.
Fresard, L. et al. Identification of rare-disease genes using blood transcriptome sequencing and large control cohorts. Nat. Med. 25, 911–919 (2019).
Posey, J. E. et al. Resolution of disease phenotypes resulting from multilocus genomic variation. N. Engl. J. Med. 376, 21–31 (2017). This retrospective analysis of exome sequence data from over 7,000 individuals found that among those with diagnostic genetic findings, nearly 5% had genetic diagnoses involving multiple disease-associated loci. These findings illustrate the importance of considering multilocus variation and using genome-wide sequencing approaches among patients whose presentation is consistent with a hereditary disease but cannot be explained by a single genetic cause.
Retterer, K. et al. Clinical application of whole-exome sequencing across clinical indications. Genet. Med. 18, 696–704 (2016).
Farwell, K. D. et al. Enhanced utility of family-centered diagnostic exome sequencing with inheritance model-based analysis: results from 500 unselected families with undiagnosed genetic conditions. Genet. Med. 17, 578–586 (2015).
Cornec-Le Gall, E., Alam, A. & Perrone, R. D. Autosomal dominant polycystic kidney disease. Lancet 393, 919–935 (2019).
Cornec-Le Gall, E., Torres, V. E. & Harris, P. C. Genetic complexity of autosomal dominant polycystic kidney and liver diseases. J. Am. Soc. Nephrol. 29, 13–23 (2018).
Porath, B. et al. Mutations in GANAB, encoding the glucosidase IIalpha subunit, cause autosomal-dominant polycystic kidney and liver disease. Am. J. Hum. Genet. 98, 1193–1207 (2016).
Cornec-Le Gall, E. et al. Monoallelic mutations to DNAJB11 cause atypical autosomal-dominant polycystic kidney disease. Am. J. Hum. Genet. 102, 832–844 (2018).
Besse, W. et al. ALG9 mutation carriers develop kidney and liver cysts. J. Am. Soc. Nephrol. 30, 2091–2102 (2019).
Lanktree, M. B., Iliuta, I. A., Haghighi, A., Song, X. & Pei, Y. Evolving role of genetic testing for the clinical management of autosomal dominant polycystic kidney disease. Nephrol. Dial. Transpl. 34, 1453–1460 (2019).
Gonzalez-Paredes, F. J., Ramos-Trujillo, E. & Claverie-Martin, F. Defective pre-mRNA splicing in PKD1 due to presumed missense and synonymous mutations causing autosomal dominant polycystic disease. Gene 546, 243–249 (2014).
Xu, P. et al. A novel splicing mutation in the PKD1 gene causes autosomal dominant polycystic kidney disease in a Chinese family: a case report. BMC Med. Genet. 19, 198 (2018).
Lanktree, M. B. et al. Intrafamilial variability of ADPKD. Kidney Int. Rep. 4, 995–1003 (2019).
Cornec-Le Gall, E. et al. Type of PKD1 mutation influences renal outcome in ADPKD. J. Am. Soc. Nephrol. 24, 1006–1013 (2013).
Hwang, Y. H. et al. Refining genotype-phenotype correlation in autosomal dominant polycystic kidney disease. J. Am. Soc. Nephrol. 27, 1861–1868 (2016).
Harris, P. C. & Torres, V. E. Polycystic kidney disease, autosomal dominant. GeneReviews https://www.ncbi.nlm.nih.gov/books/NBK1246/ (updated 19 Jul 2018).
Qian, F., Watnick, T. J., Onuchic, L. F. & Germino, G. G. The molecular basis of focal cyst formation in human autosomal dominant polycystic kidney disease type I. Cell 87, 979–987 (1996).
Reeders, S. T. Multilocus polycystic disease. Nat. Genet. 1, 235–237 (1992).
Antignac, C. et al. The future of polycystic kidney disease research–as seen by the 12 Kaplan awardees. J. Am. Soc. Nephrol. 26, 2081–2095 (2015).
Heyer, C. M. et al. Predicted mutation strength of nontruncating PKD1 mutations aids genotype-phenotype correlations in autosomal dominant polycystic kidney disease. J. Am. Soc. Nephrol. 27, 2872–2884 (2016).
Cornec-Le Gall, E. et al. The PROPKD score: a new algorithm to predict renal survival in autosomal dominant polycystic kidney disease. J. Am. Soc. Nephrol. 27, 942–951 (2016).
Iliuta, I. A. et al. Polycystic kidney disease without an apparent family history. J. Am. Soc. Nephrol. (2017).
Song, X., Haghighi, A., Iliuta, I. A. & Pei, Y. Molecular diagnosis of autosomal dominant polycystic kidney disease. Expert. Rev. Mol. Diagn. 17, 885–895 (2017).
Elisakova, V. et al. Bilineal inheritance of pathogenic PKD1 and PKD2 variants in a Czech family with autosomal dominant polycystic kidney disease — a case report. BMC Nephrol. 19, 163 (2018).
Pei, Y. et al. Bilineal disease and trans-heterozygotes in autosomal dominant polycystic kidney disease. Am. J. Hum. Genet. 68, 355–363 (2001).
Bergmann, C. et al. Mutations in multiple PKD genes may explain early and severe polycystic kidney disease. J. Am. Soc. Nephrol. 22, 2047–2056 (2011).
Cornec-Le Gall, E. et al. The value of genetic testing in polycystic kidney diseases illustrated by a family with PKD2 and COL4A1 mutations. Am. J. Kidney Dis. 72, 302–308 (2018).
Kashtan, C. E. Alport syndrome. An inherited disorder of renal, ocular, and cochlear basement membranes. Medicine 78, 338–360 (1999).
Chiereghin, C. et al. Alport syndrome cold cases: missing mutations identified by exome sequencing and functional analysis. PLoS ONE 12, e0178630 (2017).
Daga, S. et al. Urine-derived podocytes-lineage cells: a promising tool for precision medicine in Alport syndrome. Hum. Mutat. 39, 302–314 (2018).
Kamiyoshi, N. et al. Genetic, clinical, and pathologic backgrounds of patients with autosomal dominant Alport syndrome. Clin. J. Am. Soc. Nephrol. 11, 1441–1449 (2016).
Storey, H., Savige, J., Sivakumar, V., Abbs, S. & Flinter, F. A. COL4A3/COL4A4 mutations and features in individuals with autosomal recessive Alport syndrome. J. Am. Soc. Nephrol. 24, 1945–1954 (2013).
Jais, J. P. et al. X-linked Alport syndrome: natural history and genotype-phenotype correlations in girls and women belonging to 195 families: a “European community Alport syndrome concerted action” study. J. Am. Soc. Nephrol. 14, 2603–2610 (2003).
Savige, J. et al. Alport syndrome in women and girls. Clin. J. Am. Soc. Nephrol. 11, 1713–1720 (2016).
Guo, C. et al. Severe alport phenotype in a woman with two missense mutations in the same COL4A5 gene and preponderant inactivation of the X chromosome carrying the normal allele. J. Clin. Invest. 95, 1832–1837 (1995).
Rheault, M. N. et al. X-inactivation modifies disease severity in female carriers of murine X-linked Alport syndrome. Nephrol. Dial. Transpl. 25, 764–769 (2010).
Krol, R. P. et al. Somatic mosaicism for a mutation of the COL4A5 gene is a cause of mild phenotype male Alport syndrome. Nephrol. Dial. Transpl. 23, 2525–2530 (2008).
Gross, O., Netzer, K. O., Lambrecht, R., Seibold, S. & Weber, M. Meta-analysis of genotype-phenotype correlation in X-linked Alport syndrome: impact on clinical counselling. Nephrol. Dial. Transpl. 17, 1218–1227 (2002).
Jais, J. P. et al. X-linked Alport syndrome: natural history in 195 families and genotype–phenotype correlations in males. J. Am. Soc. Nephrol. 11, 649–657 (2000).
Marcocci, E. et al. Autosomal dominant Alport syndrome: molecular analysis of the COL4A4 gene and clinical outcome. Nephrol. Dial. Transpl. 24, 1464–1471 (2009).
Longo, I. et al. COL4A3/COL4A4 mutations: from familial hematuria to autosomal-dominant or recessive Alport syndrome. Kidney Int. 61, 1947–1956 (2002).
Fallerini, C. et al. Unbiased next generation sequencing analysis confirms the existence of autosomal dominant Alport syndrome in a relevant fraction of cases. Clin. Genet. 86, 252–257 (2014).
Rosado, C., Bueno, E., Felipe, C., Valverde, S. & Gonzalez-Sarmiento, R. Study of the true clinical progression of autosomal dominant Alport syndrome in a European population. Kidney Blood Press. Res. 40, 435–442 (2015).
Temme, J. et al. Incidence of renal failure and nephroprotection by RAAS inhibition in heterozygous carriers of X-chromosomal and autosomal recessive Alport mutations. Kidney Int. 81, 779–783 (2012).
Wright, C. F. et al. Assessing the pathogenicity, penetrance, and expressivity of putative disease-causing variants in a population setting. Am. J. Hum. Genet. 104, 275–286 (2019). This study examines genetic and phenotypic data from nearly 400,000 individuals to evaluate the prevalence and penetrance of putatively pathogenic variants across a variety of monogenic diseases, including type IV collagen-associated nephropathy.
Findlay, G. M. et al. Accurate classification of BRCA1 variants with saturation genome editing. Nature 562, 217–222 (2018).
Starita, L. M. et al. A multiplex homology-directed DNA repair assay reveals the impact of more than 1,000 BRCA1 missense substitution variants on protein function. Am. J. Hum. Genet. 103, 498–508 (2018).
Devuyst, O. et al. Autosomal dominant tubulointerstitial kidney disease. Nat. Rev. Dis. Prim. 5, 60 (2019).
Eckardt, K. U. et al. Autosomal dominant tubulointerstitial kidney disease: diagnosis, classification, and management — a KDIGO consensus report. Kidney Int. 88, 676–683 (2015).
Connor, T. M. et al. Mutations in mitochondrial DNA causing tubulointerstitial kidney disease. PLoS Genet. 13, e1006620 (2017).
Gomez, R. A. & Sequeira-Lopez, M. L. S. Renin cells in homeostasis, regeneration and immune defence mechanisms. Nat. Rev. Nephrol. 14, 231–245 (2018).
Bolar, N. A. et al. Heterozygous loss-of-function SEC61A1 mutations cause autosomal-dominant tubulo-interstitial and glomerulocystic kidney disease with anemia. Am. J. Hum. Genet. 99, 174–187 (2016).
Schubert, D. et al. Plasma cell deficiency in human subjects with heterozygous mutations in Sec61 translocon alpha 1 subunit (SEC61A1). J. Allergy Clin. Immunol. 141, 1427–1438 (2018).
Kirby, A. et al. Mutations causing medullary cystic kidney disease type 1 lie in a large VNTR in MUC1 missed by massively parallel sequencing. Nat. Genet. 45, 299–303 (2013). This investigation applied specialized sequencing methods to identify causal variation for MUC1-associated autosomal-dominant tubulointerstitial kidney disease, illustrating the limitations of massively parallel sequencing-based analysis alone for the diagnosis of rare monogenic disorders.
Zivna, M. et al. Noninvasive immunohistochemical diagnosis and Novel MUC1 mutations causing autosomal dominant tubulointerstitial kidney disease. J. Am. Soc. Nephrol. 29, 2418–2431 (2018).
Baigent, C. et al. Challenges in conducting clinical trials in nephrology: conclusions from a kidney disease-improving global outcomes (KDIGO) controversies conference. Kidney Int. 92, 297–305 (2017).
Breyer, M. D. & Susztak, K. Developing treatments for chronic kidney disease in the 21st century. Semin. Nephrol. 36, 436–447 (2016).
Germain, D. P. et al. Treatment of Fabry’s disease with the pharmacologic chaperone migalastat. N. Engl. J. Med. 375, 545–555 (2016). This clinical trial demonstrated that the pharmacological chaperone migalastat reduced the severity of renal, cardiac and gastrointestinal manifestations among patients with Fabry disease with responsive GLA mutations. These findings point to the importance of incorporating genotype-level knowledge when assessing the efficacy of novel therapeutic agents.
Germain, D. P. et al. Efficacy of the pharmacologic chaperone migalastat in a subset of male patients with the classic phenotype of Fabry disease and migalastat-amenable variants: data from the phase 3 randomized, multicenter, double-blind clinical trial and extension study. Genet. Med. 21, 1987–1997 (2019).
Hughes, D. A. et al. Oral pharmacological chaperone migalastat compared with enzyme replacement therapy in Fabry disease: 18-month results from the randomised phase III ATTRACT study. J. Med. Genet. 54, 288–296 (2017).
Benjamin, E. R. et al. The validation of pharmacogenetics for the identification of Fabry patients to be treated with migalastat. Genet. Med. 19, 430–438 (2017).
Ribeil, J. A. et al. Gene therapy in a patient with sickle cell disease. N. Engl. J. Med. 376, 848–855 (2017).
Adams, D. et al. Patisiran, an RNAi therapeutic, for hereditary transthyretin amyloidosis. N. Engl. J. Med. 379, 11–21 (2018).
Benson, M. D. et al. Inotersen treatment for patients with hereditary transthyretin amyloidosis. N. Engl. J. Med. 379, 22–31 (2018).
Zabaleta, N. et al. CRISPR/Cas9-mediated glycolate oxidase disruption is an efficacious and safe treatment for primary hyperoxaluria type I. Nat. Commun. 9, 5454 (2018).
Liebow, A. et al. An investigational RNAi therapeutic targeting glycolate oxidase reduces oxalate production in models of primary hyperoxaluria. J. Am. Soc. Nephrol. 28, 494–503 (2017).
Goldstein, D. B. et al. Sequencing studies in human genetics: design and interpretation. Nat. Rev. Genet. 14, 460–470 (2013).
Lek, M. et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature 536, 285–291 (2016).
Rasouly, H. M. et al. The burden of candidate pathogenic variants for kidney and genitourinary disorders emerging from exome sequencing. Ann. Intern. Med. 170, 11–21 (2019).
Ramoni, R. B. et al. The undiagnosed diseases network: accelerating discovery about health and disease. Am. J. Hum. Genet. 100, 185–192 (2017).
Rivera-Munoz, E. A. et al. ClinGen variant curation expert panel experiences and standardized processes for disease and gene-level specification of the ACMG/AMP guidelines for sequence variant interpretation. Hum. Mutat. 39, 1614–1622 (2018).
Ewans, L. J. et al. Whole-exome sequencing reanalysis at 12 months boosts diagnosis and is cost-effective when applied early in Mendelian disorders. Genet. Med. 20, 1564–1574 (2018).
Liu, P. et al. Reanalysis of clinical exome sequencing data. N. Engl. J. Med. 380, 2478–2480 (2019).
Wenger, A. M., Guturu, H., Bernstein, J. A. & Bejerano, G. Systematic reanalysis of clinical exome data yields additional diagnoses: implications for providers. Genet. Med. 19, 209–214 (2017).
Bastarache, L. et al. Phenotype risk scores identify patients with unrecognized Mendelian disease patterns. Science 359, 1233–1239 (2018). This study leveraged electronic health record data to develop phenotypic risk scores and used these scores to detect individuals with undiagnosed rare diseases, including multiple monogenic forms of kidney disease.
Wuttke, M. & Kottgen, A. Insights into kidney diseases from genome-wide association studies. Nat. Rev. Nephrol. 12, 549–562 (2016).
Torkamani, A., Wineinger, N. E. & Topol, E. J. The personal and clinical utility of polygenic risk scores. Nat. Rev. Genet. 19, 581–590 (2018).
Liu, L. & Kiryluk, K. Genome-wide polygenic risk predictors for kidney disease. Nat. Rev. Nephrol. 14, 723–724 (2018).
Martin, A. R. et al. Clinical use of current polygenic risk scores may exacerbate health disparities. Nat. Genet. 51, 584–591 (2019). This incisive commentary discusses how the variable performance of genome-wide polygenic risk scores across different ethnic groups could exacerbate existing health disparities, highlighting the need to prioritize greater diversity in genetic research.
Mostafavi, H. et al. Variable prediction accuracy of polygenic scores within an ancestry group. eLife 9, e48376 (2020).
Acknowledgements
The work of the authors is supported by grants from the US National Institutes of Health (1F30DK116473 (E.E.G.) and 2R01DK080099, R01DK082753 and U54DK104309 (A.G.G.)).
Author information
Authors and Affiliations
Contributions
All authors contributed substantially to the research and writing process, including discussing the content of the article and reviewing and editing the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
A.G.G. has served as a consultant for the AstraZeneca Center for Genomics Research and for Goldfinch Bio. The other authors declare no competing interests.
Additional information
Peer review information
Nature Reviews Nephrology thanks R. Gbadegesin, A. Mallett and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
ClinGen: https://clinicalgenome.org/
DECIPHER: https://decipher.sanger.ac.uk/
Supplementary information
Glossary
- Heritability
-
The proportion of interindividual variation in a trait that is caused by genetic factors.
- Private variants
-
Genetic variants unique to a single individual (that is, variants not observed in other individuals).
- Phenocopy
-
A phenotype that bears resemblance to the phenotype resulting from a particular genotype but occurs in an individual who does not harbour that genotype.
- Pleiotropy
-
Variation in a single gene influencing multiple phenotypic traits.
- Incomplete penetrance
-
Penetrance is the proportion of individuals with a particular genotype who display the associated phenotype. In the case of incomplete penetrance, not all individuals with the genotype manifest the associated phenotype.
- Variable expressivity
-
Expressivity refers to the extent to which individuals with a given genetic disease display the associated phenotype and thus reflects the range of phenotypes associated with the genotype. Variable expressivity describes a situation wherein affected individuals display the associated phenotype to differing extents.
- Papillorenal syndrome
-
Also known as renal coloboma syndrome. A disorder resulting from pathogenic variants in PAX2 characterized by kidney disease and ophthalmological anomalies; other manifestations may include sensorineural hearing loss, soft skin and ligamentous laxity.
- Oligogenic inheritance
-
A form of inheritance in which transmission of a phenotypic trait is mediated by multiple different genetic loci.
- Digenic inheritance
-
A form of inheritance in which transmission of a phenotypic trait is mediated by two different genetic loci.
- Structural variants
-
Large (≥1-kb) DNA variants; these alterations can be balanced (for example, inversions or reciprocal translocations, with no overall change in the amount of DNA at the relevant locus) or imbalanced (for example, copy number variants), which lead to gain or loss of DNA at the relevant locus.
- Single nucleotide variants
-
Alterations of single bases (nucleotides) in a DNA sequence; single nucleotide variants can lead to a different amino acid sequence in the encoded protein (non-synonymous variants) or leave the sequence unchanged (synonymous variants).
- Insertions or deletions
-
Gains or losses in the number of bases in a DNA sequence versus the reference sequence at that site, producing a different amino acid sequence in the encoded protein.
- Copy number variants
-
(CNVs). Structural variants that lead to gain (duplications) or loss (deletions) of DNA at the relevant locus.
- Genic copy number variants
-
Copy number variants that contain protein-coding regions of the genome (that is, genes).
- Locus
-
A specific site in the genome (plural: loci).
- Haploinsufficiency
-
A condition resulting from inactivation of one copy of a gene for which two copies are needed for normal gene function; for such haploinsufficient genes, gene function is thus altered in heterozygotes, as the remaining (functional) copy does not produce sufficient gene product for normal function.
- Meiotic non-allelic homologous recombination
-
Exchange of genetic material (DNA) between homologous regions located on different loci during meiosis.
- Epistatic interactions
-
Interaction between multiple different loci, wherein the phenotypic impact of the genotype at one locus depends on the genotype at other loci.
- Mobile genetic elements
-
DNA sequences that can move from their original site and integrate into another, different region of the genome
- Retrotransposition
-
Insertion of a DNA sequence at a new site in the genome using an RNA intermediate: the DNA sequence is first transcribed into RNA, and the RNA is then reverse transcribed into DNA, which is then inserted at the new site.
- Mosaic variants
-
Genetic variants that are present in a mosaic form — that is, the genotype at that locus is present within a certain proportion of an individual’s cells, such that they have multiple genetically different cell populations, with different genotypes at that locus.
- Pseudohomology
-
The state in which the DNA sequence of a (protein-coding) gene is highly similar to the DNA sequence of a pseudogene (that is, a copy of the gene that is not transcribed or translated, and thus does not yield a protein), because they both originate from the same ancestral gene.
- Synonymous variants
-
DNA sequence changes in the protein-coding (exonic) regions of the genome that do not alter the amino acid in the associated encoded proteins.
- Sanger sequencing
-
A method of DNA sequencing that uses labelled chain-terminating dideoxynucleotides to detect the nucleotides in the DNA strand being sequenced. This method yields a sequence chromatogram, which can subsequently be analysed to identify genetic variants.
- Sequencing coverage and read depths
-
In this Review, sequencing coverage refers to the percentage of bases in the DNA region targeted by sequencing that is sequenced a given number of times. Sequencing depth denotes the average number of times that a given nucleotide is read in a set of DNA sequence reads. Higher coverage and depth means that more of the targeted genomic region has been sampled a greater number of times, increasing the technical accuracy of the resulting data.
- Hemizygous
-
The condition in which an individual has a single copy of a pair of chromosomes or a segment of a chromosome pair, rather than two copies. This occurs for genes located on the X chromosome among human males, as their sex chromosomes comprise one X chromosome and one Y chromosome
- Saturation editing
-
A technique that replaces a DNA sequence in a gene of interest with variant DNA sequences encoding alternative amino acids in order to generate all possible amino acid substitutions at that site in the protein. The impact of each of the mutations on wild-type (non-mutated/normal) protein function can then be evaluated through various high-throughput screening assays (for example, for a gene encoding a kinase enzyme, assessing its ability to phosphorylate its substrate).
- Transthyretin amyloidosis
-
A disorder resulting from systemic amyloid deposition in organs including the heart, liver, nervous system and kidney owing to mutations in TTR.
Rights and permissions
About this article
Cite this article
Groopman, E.E., Povysil, G., Goldstein, D.B. et al. Rare genetic causes of complex kidney and urological diseases. Nat Rev Nephrol 16, 641–656 (2020). https://doi.org/10.1038/s41581-020-0325-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41581-020-0325-2
This article is cited by
-
Frequency, morbidity and equity — the case for increased research on male fertility
Nature Reviews Urology (2024)
-
Genetics of SLE: mechanistic insights from monogenic disease and disease-associated variants
Nature Reviews Nephrology (2023)
-
The genetic basis of congenital anomalies of the kidney and urinary tract
Pediatric Nephrology (2022)
-
Evolutionary genetics and acclimatization in nephrology
Nature Reviews Nephrology (2021)
-
An accessible insight into genetic findings for transplantation recipients with suspected genetic kidney disease
npj Genomic Medicine (2021)