Abstract
Gestational diabetes mellitus (GDM) is of public health concern. This trial examined whether a clinically proven lifestyle modification program (LMP) in early pregnancy was superior to routine antenatal care in improving GDM, maternal and infant outcomes. Chinese pregnant women at risk of GDM (n = 220) were recruited at or before 12-week gestation and randomized to either a LMP group or a routine care control group. Eighty subjects completed a dietitian-led LMP including dietary and exercise components from early pregnancy till 24-week gestation. Data were compared with those of 86 control subjects. Twenty three (26.7%) control subjects and 20 (25.0%) LMP subjects developed GDM (p = 0.798). The proportion of infants born large for gestational age and macrosomia was similar between groups. The LMP group showed a lower proportion of excessive gestational weight gain (GWG). Subgroup analysis suggested that those with higher LMP adherence showed more desirable dietary composition and energy intake, and lower proportion of excessive GWG compared with the low LMP adherence group and the control group. The potential effect of LMP on GDM and other maternal and infant outcomes, in particular GWG, as well as barriers for making lifestyle changes warrant further investigations (ClinicalTrials.gov NCT02368600).
Similar content being viewed by others
Introduction
Gestational diabetes mellitus (GDM) is defined as a type of diabetes first diagnosed during pregnancy1. With increasing prevalence of obesity and diabetes worldwide, the number of women with GDM is also increasing2. Women with GDM have an increased risk developing metabolic syndrome3 and vascular diseases4. GDM has also been linked with higher rates of cesarean sections, induced deliveries, shoulder dystocia and macrosomia, as well as predisposes the offspring to overweight and metabolic syndrome4,5. These observations highlight the importance of timely intervention in the prenatal period in reducing the lifetime burden from non-communicable diseases.
Currently there is no consensus regarding the best intervention for weight management and GDM reduction during pregnancy6. Available evidence appears to suggest that antenatal lifestyle interventions, especially dietary interventions are associated with restricted gestational weight gain (GWG) and could possibly reduce the risk of GDM in overweight or obese pregnant women7. However, most available trials that have been conducted in Western and Chinese populations focused on the treatment of GDM and only few of them have tested the effectiveness of lifestyle interventions using the prevention of GDM as the primary outcome8,9. Therefore, well designed randomized trials with standardized behavioural interventions are warranted.
This trial examined the potential use of a clinically proven lifestyle modification program (LMP)10,11 in early pregnancy in preventing GDM in Chinese pregnant women at high risk of GDM in Hong Kong. The proposed intervention was unique that it was offered at or before 12 weeks of gestation, and such design supported the importance of early intervention in pregnancy in reducing GDM and preventing excessive GWG. We aimed to compare the effectiveness of a lifestyle intervention in early pregnancy with usual antenatal care in reducing the GDM incidence (primary outcome), decreasing the proportion of infants born large for gestational age (LGA) and being classified as macrosomia (secondary outcomes), as well as improving other maternal and birth outcomes (tertiary outcomes) in Chinese pregnant women at risk of GDM in Hong Kong. We hypothesized that the proposed lifestyle invention was superior to usual antenatal care in improving all these outcomes.
Materials and Methods
Study design and study population
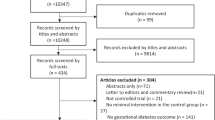
This was a prospective parallel group, single-blind randomized controlled trial (RCT), which was conducted between April 2015 and April 2017 (Supplement 1). Chinese women with age of 18 years old and above and having a gestational age <=12 weeks were recruited using a convenience sampling method at the antenatal clinic of a study hospital in Hong Kong. Research staff screened clients attending the clinic and identified eligible participants.
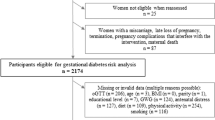
Women should fulfil at least one of the hospital criteria of defining as at risk of GDM upon recruitment. The criteria included maternal age >=35 years old at the expected date of confinement; prior history of GDM or birth of child >=4 kg; pre-pregnant body mass index (BMI) or BMI at the 1st trimester >=25 kg/m2; and family history of diabetes at the first degree relatives. Those who were participating in any clinical trial, had pre-existing diabetes, multiple pregnancies, substance abuse, renal, liver or thyroid dysfunction, cognitive impairment, or any other indication of major medical or psychological illnesses, as well as physical restriction that led to exercise avoidance were excluded. All participants provided written informed consent. The study protocol was performed in compliance with the Declaration of Helsinki and was approved by the Clinical Research Ethics Committee of The Chinese University of Hong Kong. The study was registered at ClinicalTrials.gov (NCT02368600, registered date: 15/02/2015).
Eligible participants were randomized in 1:1 ratio to either the intervention group or the control group upon recruitment. Randomization was performed through the use of a computer-generated list of random numbers in blocks of 6 by a study coordinator. Treatment assignments were concealed in consecutively-numbered sealed envelopes, which were opened sequentially upon subject enrollment. The interventionists (the dietitian and the exercise instructor), the participants and the study coordinator were not blinded to the treatment assignment. However, the interventionists did not take any outcome measurements. All investigators, outcome assessors, clinicians and nurses of routine antenatal and postnatal care were blinded to the treatment assignment.
Intervention group (LMP group)
On top of routine antenatal care, participants in the intervention group participated in a dietitian-led lifestyle intervention from the first antenatal booking (i.e. <=12 weeks of gestation) to 24 weeks of gestation. The intervention was designed based on a clinically proven LMP11. Participants received bi-weekly face-to-face or phone consultations in the first 2 months and monthly face-to-face consultations afterwards till the end of the intervention (i.e. 24–28 weeks of gestation). At the first 1-hour face-to-face session, the dietitian comprehensively reviewed the participant’s lifestyle habits, medical, pregnant and birth history, as well as the fetal growth status and the participant’s weight gain of current pregnancy, and discussed the specific dietary and lifestyle advices to achieve a desirable weight status with the participant. In the follow-up consultations through face-face interviews or phone calls (~20 minutes), the dietitian reviewed the participant’s dietary and lifestyle practices and provided recommendations. Each participant was given an individualized menu plan and healthy lifestyle booklets aiming at achieving a varied balanced diet with an emphasis on fruit and vegetables consumption, and intake of moderate-carbohydrate, low-fat, low-glycemic index (GI) and low-calorific products in appropriate portions. The diet plan was also designed to achieve a desirable fetal growth and maternal weight throughout pregnancy. Advice on the use of dietary supplements and managing pregnancy discomforts was given. Participants could email their enquiries to the dietitian.
Besides, participants were encouraged to see the exercise instructor at least once during the LMP. During the exercise consultation (~30 minutes), the exercise instructor reviewed participant’s medical history as well as pre-pregnant and current exercise habits, assessed participant’s fitness level and musculoskeletal problems, and designed a suitable exercise regime for the participant based on international guidelines12,13. Participants were generally advised to do a 30-minute of easy to moderate intensity of low impact aerobic exercise at least three times a week.
Control group
The control group received routine antenatal care. In brief, body weight of pregnant woman attending the antenatal clinic was monitored at each antenatal visit by nurses. Educational booklet on diet and exercise recommendations during pregnancy was delivered to them. They were also offered optional antenatal classes which were subjected to the class availability.
Study outcomes and sample size calculation
The primary outcome was the proportion of participants in each group with GDM at 24–28 weeks of gestation. The secondary outcomes included the proportion of neonates born with LGA (>90th percentile of the customized birth weight) and macrosomia (>=4 kg at birth).
Sample size was calculated based on the primary outcome using data from a previous trial14. A sample size of 73 per group was calculated with power of 90% at a 1% alpha level and two-sided test to detect an 83% reduction in the odds of decreased GDM in the intervention group when compared with the control group14. Assuming 30% lost to follow-up rate and 5% miscarriage rate, a final sample size of 110 participants per group was decided.
Measurements
Maternal and fetal/neonatal data were collected by trained research staff at different stages of pregnancy, after delivery and 6–8 weeks postpartum. A cash of HK$50 (i.e. about 6 US dollars) was given to the participants for the completion of assessments at designated time points.
Data on demographics, lifestyle habits, as well as medical and obstetric history were collected using a standardized questionnaire at baseline (i.e. <=12 weeks of gestation). Maternal weight, height and blood pressure were measured using standardized methods at various time points, and pre-pregnant weight was self-reported. The total GWG was calculated as the difference in the weight measured on the day of delivery and the self-reported pre-pregnant weight.
A 3-day diet record was used to assess subject’s diet at baseline and 24–28 weeks of gestation. Daily nutrient intake and consumption of food group of each subject were calculated using the nutrition analysis software Food Processor Nutrition analysis and Fitness software version 8.0 (ESHA Research, Salem, USA) which included nutrient data of local foods from food composition tables from China and Hong Kong. Since no validated Chinese questionnaire for measuring physical activity level for pregnant women was available, the Chinese version of the International Physical Activity Questionnaire (IPAQ-C)15 was used to assess the physical activity level. A diet adherence score and a physical activity adherence score were generated based on the 3-day diet record and the IPAQ-C respectively for the participants in the LMP group at baseline and 24–28 weeks of gestation. The diet adherence score consisted of eight criteria and one score was given for meeting each of the criteria: (i) total energy not exceeding 10% of the diet plan; (ii)% energy from fat 20–30%; (iii)% energy from protein within the range of 15–20%; (iv)% energy from carbohydrate 50–60%; (v) consumption of fruit ≥160 g; (vi) consumption of vegetables ≥240 g; (vii) regular meal consumption and (viii) “Avoid food (e.g. high fat or high sugar foods/GI foods)” not being consumed. The total score ranged from 0 to 24 for each time point. Adherence to the LMP was also assessed based on the percentage attendance to the proposed LMP sessions. The physical activity adherence score was assessed based on the IPAQ-C data. Two scores were given if 80% of the recommended volume of exercise (frequency x duration) was met during the week of follow-up (7 days) while one score was given if 50% of the recommended volume of exercise was achieved. Zero score was given for those who did not perform any easy to moderate intensity of low impact aerobic exercise. Number of exercise consultation sessions attended by the participants was also documented.
Participants in the intervention group were asked to rate the perceived support from the dietitian and the exercise instructor at 24–28 weeks of gestation using the validated Chinese version of Health Care Climate Questionnaire (HCCQ)16. HCCA is a 15-item patient-rated measure related to the perceived supportiveness of health care providers. Each item has a scale of 1 (strongly disagree) to 7 (strongly agree). A total rated score can be generated with a range of 1 (lowest perceived support) to 7 (highest perceived support). A higher rated total score indicates higher perceived support.
A 75 g 2-h oral glucose tolerance test (OGTT) was done at 24–28 weeks of gestation on routine care basis. GDM was diagnosed using the modified World Health Organization criteria in which one or more of the criteria were met: (i) fasting plasma glucose 5.1–6.9 mmol/L; (ii) 1-hour plasma glucose >=10 mmol/L; or (iii) 2-hour plasma glucose 8.5–11.0 mmol/L following a 75 g oral glucose load17. OGTT was repeated at 6–8 weeks postpartum for those who had GDM at 24–28 weeks of gestation.
Perinatal and obstetric outcomes, neonatal outcomes and complications were retrieved from the hospital record. Perinatal and obstetric outcomes and complications included preeclampsia, gestational hypertension, Caesarean section and preterm delivery, and gestation at delivery (week). Fetal and neonatal outcomes included Apgar score at 5 minutes, neonatal weight, small for gestational age (SGA), LGA, macrosomia, and shoulder dystocia.
Data analysis
Data were presented as mean (standard deviation, SD) for normally distributed variables, median (interquartile range, IQR) for skewed variables and frequency (percentage) for categorical variables where appropriate. Between-groups comparisons at baseline and after intervention were made using the Student’s t test, Chi-square test or Fisher’s exact test where appropriate. Data were analysed using both the intention-to-treat (ITT) approach and the per-protocol (PP) approach. The compliance to the LMP protocol were assessed based on the adherence scores and the attendance data. Those who achieved at least 50% of the diet adherence score as well as attending at least 70% of the dietetic consultations and at least one exercise consultation were defined as high LMP adherent cases for the PP analysis. The physical activity adherence score was finally excluded from the criteria for PP analysis because majority of the LMP participants had zero physical activity adherence score. Regression techniques were used to examine the influence of prognostic factors on the major outcomes. Multivariate regression models including logistic regression, linear regression, analysis of covariance, and multinomial regression were used to compare differences between the 2 groups for all measured outcomes at baseline and 24–28 weeks of gestation or at delivery with adjustment for potential covariates. Potential covariates included maternal age (continuous), marital status (married vs. others), family monthly income (less than HK$ 20,000 vs. HK$ 20,000 or above), and pre-pregnant BMI (continuous). They were mainly chosen based on p < 0.2 in the univariate analysis. All statistical tests were two-sided and a p-value < 0.05 was considered statistically significant. SPSS for Windows software (version 24.0, SPSS Inc., Chicago, IL, USA) was used for the statistical analysis.
Results
Characteristics of the participants
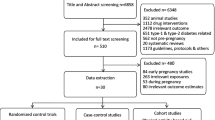
Figure 1 shows the number of participants at different study stages. Participants who were classified as loss to follow-up or drop out (n = 26) were more likely to be ex-smokers (n = 5, 19.2%) in comparison to those who remained in the study (n = 11 out of 194, 5.7%) (p = 0.027). The mean (SD) age and BMI of the final 166 participants were 33.1 (4.2) years and 23.6 (4.0) kg/m2 respectively. The gestational age at enrolment ranged from 4 to 11 weeks and 59.6% of them were nulliparous. Baseline characteristics were comparable between the two study groups (Table 1).
Compliance of the LMP group
Overall, 93.8% participants attended at least 70% of the dietetic consultations and 92.5% participants attended at least one exercise consultation. Diet adherence score ranged from 2 to 18, with mean (SD) of 9 (3). Physical activity adherence score ranged from 0 to 2, with median (IQR) of 0 (0-0). Mean (SD) scores of perceived support from the dietitian and the exercise instructor were 5.8 (0.6) and 5.4 (0.7) respectively. Fourteen participants in the LMP group were classified as high LMP adherence group and they were included for PP analysis.
Dietary intakes were similar between the two groups (Table 2). The magnitude of increase in energy intake was however significantly smaller in the LMP group than the control group. The high LMP adherence group also showed a significantly smaller magnitude of increase in energy intake than the control group in the PP analysis. The high LMP adherence group showed a trend of adopting a more balanced diet in terms of the energy contribution from various macronutrients (i.e. reduced percentage energy from total fat and saturated fat) after the intervention compared with the control group (Table 3). In subgroup analysis, the high LMP adherence group shifted to a more balanced diet (i.e. reduced percentage energy from total fat and saturated fat) compared with the low LMP adherence group, although the magnitude of increase in energy intake was similar between the two groups (details not shown).
Baseline physical activity level was similar between the LMP group and the control group. Walking accounted for the majority of daily physical activities in both groups. There was no significant between-group difference in the change of physical activity variables (Table 2). Similar results were observed for the PP analysis (Table 3). Subgroup analysis showed no significant difference in the physical activity variables between the high LMP adherence group and the low LMP adherence group (details not shown).
Study outcomes
There was no significant difference in the GDM incidence and the total GWG between the LMP group and the control group. No significant difference in LGA, macrosomia and other maternal and infant outcomes was observed between the two groups (Table 4). However, pre-pregnant BMI was found to be a significant factor for both the GDM incidence and the total GWG in the adjusted models (details not shown). Higher pre-pregnant BMI was associated with higher risk of GDM incidence [OR (95% CI): 1.12 (1.02 to 1.23), p = 0.022] and lower total GWG [Beta (95% CI): −0.426 (−0.631 to −0.220), p < 0.001].
Among the 43 subjects who developed GDM at 24–28 weeks of gestation, thirty-nine (19 LMP, 20 control) repeated OGTT at 6–8 weeks postpartum. There were 9 (45%), 4 (20%) and 7 (35%) subjects in the control group with normal glucose, impaired fasting glucose and impaired glucose tolerance status respectively whereas the number (%) was 8 (42.1%), 5 (26.3%) and 6 (31.6%) respectively in the LMP group (p = 0.895).
Although there were no significant differences in the rates of GDM and most outcomes between the high LMP adherence group and the control group, the former showed a significantly better control in the total GWG than the latter in both the crude and adjusted models (Table 5). Similarly, most study outcomes were not affected by the LMP adherence. However, the high LMP adherence group tended to show a lower proportion of excessive GWG compared with the low LMP adherence group (0% vs. 21.3%, p = 0.099) (details not shown).
Discussion
Our study is one of the few available studies among Chinese pregnant women to examine the effectiveness of a lifestyle intervention in early pregnancy on GDM prevention. Unexpectedly, we failed to show any significant difference in any measured outcomes between the LMP group and the control group. Only a non-significant trend in limiting excessive GWG was observed in the LMP group. Our results were different from those reported by Sun and colleagues9 but consistent with the findings from other groups18,19,20,21 Sun et al. examined the effectiveness of a lifestyle intervention in early pregnancy on GDM prevention in 74 Chinese overweight and obese women (i.e. BMI >=24 kg/m2)9. The intervention included counselling sessions on diet, exercise and pregnant weight gain delivered by the research nurse at recruitment and on monthly basis in the second trimester plus weekly follow-up phone calls or emails between antenatal visits. The control group only received the same counselling at recruitment delivered by the research nurse and routine health education in the clinic. Lower incidence of GDM and lower excessive weight gain at the end of the second trimester were observed in the intervention group in comparison to the control group9. In contrast, other studies showed that lifestyle interventions did not alter the risk of GDM. A cluster RCT in Finland showed that individual intensive counselling on diet, physical activity and weigh gain offered by a nurse to pregnant women with at least one GDM risk factor within 8–12 weeks of gestation was effective in controlling neonatal birthweight and LGA but failed to reduce maternal GDM or limit GWG compared with the usual care control group. However, those who highly adhered to the intervention showed decreased risk of GDM and lower proportion of infants born with LGA compared with the usual care control group. About 60% of the overall sample in this Finnish study was overweight (i.e. BMI >25 kg/m2) at baseline18. In another RCT examining the effect of a lifestyle intervention including two phone dietary consultations and twice-weekly exercise groups on glucose metabolism in 606 healthy first time pregnant women with pre-pregnant BMI > = 19 kg/m2, the intervention failed to improve glucose levels or reduce GDM incidence but was able to reduce GWG at term as well as the insulin and leptin levels20. Similar lack of effect of lifestyle interventions on GDM prevention have been reported in other studies. However, the effectiveness of lifestyle interventions on other outcomes, such as limiting GWG or reducing proportion of infants born with LGA remains uncertain19,21.
Of particular interest is that those with higher adherence to the LMP in the present study showed a more desirable dietary energy intake and composition, and a lower proportion of excessive total GWG as compared with the control group and the low LMP adherence group. Meanwhile, low LMP adherence warrants concern. Although LMP participants reported a moderate to high perceived support from both dietitian and exercise instructor, previous studies suggested that some personal, social and environmental factors, such as social support, working environment and availability of healthy food choices may influence one’s food choices and physical activity behaviour during the lifestyle intervention11,22. Our observations possibly suggest that the LMP is potentially beneficial for bringing dietary changes only in those who have high motivation for lifestyle changes. Whether such lifestyle changes could lead to an ultimate reduction in the GDM incidence may require a trial with a larger sample size. Further studies are needed to identify barriers and best strategies to facilitate lifestyle changes in this high risk group.
Several reasons possibly explain the absence of effect of the LMP on the expected outcomes in our study. First, we recruited pregnant women at risk of GDM based on the hospital criteria and the average BMI at entry was about 23 kg/m2. Approximately 40% of them were overweight or obese at the time of enrolment. In contrast, other studies which were able to demonstrate the effectiveness of lifestyle interventions in reducing GDM incidence, limiting GWG or improving other maternal and neonatal outcomes mainly targeted overweight or obese women with pre-pregnant BMI of at least 24 kg/m2. Whether the LMP could produce a more pronounced effect on the outcomes in overweight or obese pregnant women remains to be explored. Second, the observed difference in GDM incidence between the LMP group and the control group for sample size calculation was smaller than expected. In contrast, the observed 12% miscarriage rate in the study was higher than that (i.e. 5%) used in the sample size calculation, thus the study may be underpowered. Third, the physical activity data showed that the exercise component of the LMP may need to be strengthened. Previous studies showed that supervised exercise programs might reduce GDM incidence23,24, limit GWG23, as well as improve some maternal and neonatal outcomes24,25. However, in traditional Chinese culture, pregnancy is considered as a vulnerable period that requires rest and protection. These cultural beliefs have been reported as the major barriers for increasing physical activity level in Chinese pregnant women26,27. However, our study findings showed that physical activity level was generally low among Chinese pregnant women in Hong Kong. More importantly, our findings revealed that giving advice on physical activity alone by the exercise instructor in the LMP did not produce increased physical activity level among the LMP participants. In view of the findings, a more intensive physical activity component, such as the possibility of supervised exercise programs or groups could be considered in the LMP as to pose some more impacts on the measured outcomes. However, the intensity, types and frequency of the exercise program, and the best model of delivery of the exercise program as well as the target group that would benefit most from the exercise program in terms of the local context remain to be identified. Fourth, consistent with the findings from previous studies that higher pre-pregnant BMI was associated with higher risk of GDM incidence and lower total GWG, whether the intervention approach should start before pregnancy warrants further investigation.
Our study has several limitations. First, the recruitment was done in one hospital and the results may not be generalized. Second, there is no routine measurement of infant’s length and head circumference at birth in the study hospital, and some mother-infant pairs had been discharged from the hospital prior to the anthropometric measurement by the research team. Therefore, anthropometric data of some infants were missing. Third, some mothers chose to give birth in the private hospital, thus most birth and infant data of these mothers were self-reported by the mothers based on the available record from the private hospital. Fourth, absence of any difference in most outcomes between the two groups might be due to the inadequate sample size used. Last, the IPAQ used was not specifically designed for pregnant population. Other feasible methods, such as the use of accelerometer for measuring physical activity among pregnant women may be more accurate.
In conclusion, the LMP proposed in the study did not influence GDM risk and other maternal and infant outcomes in Chinese pregnant women at risk of GDM in Hong Kong. Pregnant women with higher adherence to the LMP showed a more desirable dietary composition and energy intake, and a lower proportion of excessive GWG. The potential effect of the LMP on improving maternal outcomes, in particular GWG, may require study with a larger sample size and stronger exercise component. Barriers for Chinese pregnant women in Hong Kong to make lifestyle changes and best strategies to faciliate such changes also warrant further investigations.
Data Availability
All data generated or analysed in the study are included in this published article.
References
Metzger, B. E. Summary and recommendations of the Third International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes. 40, S197–201 (1991).
Roglic, G. Diabetes in women: the global perspective. Int J Gynaecol Obstet. 104, S11–13 (2009).
Tam, W. H. et al. Cardiometabolic risk in Chinese women with prior gestational diabetes: a 15-year follow-up study. Gynecol Obstet Invest. 73, 168–176 (2012).
Kaaja, R. & Rönnemaa, T. Gestational Diabetes: Pathogenesis and Consequences to Mother and Offspring. Rev Diabet Stud. 5, 194–202 (2008).
Tam, W. H. et al. Glucose intolerance and cardiometabolic risk in adolescents exposed to maternal gestational diabetes: a 15-year follow-up study. Diabetes Care. 33, 1382–1384 (2010).
Thangaratinam, S. et al. Effects of interventions in pregnancy on maternal weight and obstetric outcomes: meta-analysis of randomised evidence. BMJ. 344, e2088 (2012).
Oteng-Ntim, E., Varma, R., Croker, H., Poston, L. & Doyle, P. Lifestyle interventions for overweight and obese pregnant women to improve pregnancy outcome: systematic review and meta-analysis. BMC Med. 10, 47 (2012).
Xu, T. et al. Healthcare interventions for the prevention and control of gestational diabetes mellitus in China: a scoping review. BMC Pregnancy Childbirth. 17, 171 (2017).
Sun, Y. & Zhao, H. The effectiveness of lifestyle intervention in early pregnancy to prevent gestational diabetes mellitus in Chinese overweight and obese women: A quasi-experimental study. Appl Nurs Res. 30, 125–130 (2016).
Woo, J. et al. Effectiveness of a lifestyle modification programme in weight maintenance in obese subjects after cessation of treatment with Orlistat. J Eval Clin Pract. 13, 853–859 (2007).
Chan, R. S., Lok, K. Y., Sea, M. M. & Woo, J. Clients’ experiences of a community based lifestyle modification program: a qualitative study. Int J Environ Res Public Health. 6, 2608–2622 (2009).
Artal, R. & O’Toole, M. Guidelines of the American College of Obstetricians and Gynecologists for exercise during pregnancy and the postpartum period. Br J Sports Med. 37, 6–12 (2003).
Canadian Society for Exercise Physiology. Physical activity readiness medical examination. http://www.csep.ca/cmfiles/publications/parq/parmed-xpreg.pdf (2013).
Quinlivan, J. A., Lam, L. T. & Fisher, J. A randomised trial of a four-step multidisciplinary approach to the antenatal care of obese pregnant women. Aust N Z J Obstet Gynaecol. 51, 141–146 (2011).
Macfarlane, D. J., Lee, C. C., Ho, E. Y., Chan, K. L. & Chan, D. T. Reliability and validity of the Chinese version of IPAQ (short, last 7 days). J Sci Med Sport. 10, 45–51 (2007).
Chan, D. K. C., Hagger, M. S. & Spray, C. M. Treatment motivation for rehabilitation after a sport injury: Application of the trans-contextual model. Psychol Sport Exerc. 12, 83–92 (2011).
World Health Organization. Diagnostic Criteria and Classification of Hyperglycaemia First Detected in Pregnancy. Geneva: World Health Organization, 2013.
Luoto, R. et al. Primary prevention of gestational diabetes mellitus and large-for-gestational-age newborns by lifestyle counseling: a cluster-randomized controlled trial. PLoS Med. 8, e1001036 (2011).
Bruno, R. et al. Adherence to a lifestyle programme in overweight/obese pregnant women and effect on gestational diabetes mellitus: a randomized controlled trial. Matern Child Nutr. 13, 12333 (2017).
Sagedal, L. R. et al. The effect of a prenatal lifestyle intervention on glucose metabolism: results of the Norwegian Fit for Delivery randomized controlled trial. BMC Pregnancy Childbirth. 17, 167 (2017).
Simmons, D. et al. Effect of Physical Activity and/or Healthy Eating on GDM Risk: The DALI Lifestyle Study. J Clin Endocrinol Metab. 102, 903–913 (2017).
O’Brien, O. A. et al. Influences on the food choices and physical activity behaviours of overweight and obese pregnant women: A qualitative study. Midwifery. 47, 28–35 (2017).
Wang, C. et al. Effect of Regular Exercise Commenced in Early Pregnancy on the Incidence of Gestational Diabetes Mellitus in Overweight and Obese Pregnant Women: A Randomized Controlled Trial. Diabetes Care. 39, e163–164 (2016).
Garnaes, K. K., Morkved, S., Salvesen, O. & Moholdt, T. Exercise Training and Weight Gain in Obese Pregnant Women: A Randomized Controlled Trial (ETIP Trial). PLoS Med. 13, e1002079 (2016).
Embaby, H., Elsayed, E. & Fawzy, M. Insulin Sensitivity and Plasma Glucose Response to Aerobic Exercise in Pregnant Women at Risk for Gestational Diabetes Mellitus. Ethiop Journal Health Sci. 26, 409–414 (2016).
Zhang, Y. et al. Physical activity level of urban pregnant women in Tianjin, China: a cross-sectional study. PLoS One. 9, e109624 (2014).
Guelfi, K. J. et al. A comparison of beliefs about exercise during pregnancy between Chinese and Australian pregnant women. BMC Pregnancy Childbirth. 15, 345 (2015).
The American College of Obstetricians and Gynecologists. The American College of Obstetricians and Gynecologists Committee opinion no. 548: weight gain during pregnancy. Obstet Gynecol. 121, 210–212 (2013).
Acknowledgements
The project was funded by a grant from the Health and Medical Research Fund, Food and Health Bureau, Hong Kong SAR Government (Ref no: 12130061). The authors gratefully acknowledge and thank the Health and Medical Research Fund and the University Grants Council for funding the research project. The authors also thank all the participants in the study.
Author information
Authors and Affiliations
Contributions
R.S.M.C. designed the study. W.H.T., M.M.M.S. and J.W. provided advice on the study design and implementation. I.C.H.H., M.W.C.K. and L.S.L. performed the study and collected the study data. R.S.M.C. performed data analysis and wrote the main manuscript text. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chan, R.SM., Tam, WH., Ho, I.CH. et al. Randomized trial examining effectiveness of lifestyle intervention in reducing gestational diabetes in high risk Chinese pregnant women in Hong Kong. Sci Rep 8, 13849 (2018). https://doi.org/10.1038/s41598-018-32285-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-32285-6
Keywords
This article is cited by
-
Interventions in preconception and pregnant women at risk of gestational diabetes; a systematic review and meta-analysis of randomised controlled trials
Diabetology & Metabolic Syndrome (2024)
-
Mapping Lifestyle Interventions for Gestational Diabetes Prevention: A Scoping Review
Current Diabetes Reports (2024)
-
Effective interventions in preventing gestational diabetes mellitus: A systematic review and meta-analysis
Communications Medicine (2024)
-
Lifestyle intervention in early pregnancy can prevent gestational diabetes in high-risk pregnant women in the UAE: a randomized controlled trial
BMC Pregnancy and Childbirth (2022)
-
Recurrent gestational diabetes
Wiener klinische Wochenschrift (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.