Abstract
Injury to podocytes is a principle cause of initiation and progression of both immune and non-immune mediated glomerular diseases that result in proteinuria and decreased function of the kidney. Current advances in regenerative medicine shed light on the therapeutic potential of cell-based strategies for treatment of such disorders. Thus, there is hope that generation and transplantation of podocytes from induced pluripotent stem cells (iPSCs), could potentially be used as a curative treatment for glomerulonephritis caused by podocytes injury and loss. Despite several reports on the generation of iPSC-derived podocytes, there are rare reports about successful use of these cells in animal models. In this study, we first generated a model of anti-podocyte antibody-induced heavy proteinuria that resembled human membranous nephropathy and was characterized by the presence of sub-epithelial immune deposits and podocytes loss. Thereafter, we showed that transplantation of functional iPSC-derived podocytes following podocytes depletion results in recruitment of iPSC-derived podocytes within the damaged glomerulus, and leads to attenuation of proteinuria and histological alterations. These results provided evidence that application of iPSCs-derived renal cells could be a possible therapeutic strategy to favorably influence glomerular diseases outcomes.
Similar content being viewed by others
Introduction
Nephrotic syndrome (NS), as a hallmark of glomerular disease (GD), is characterized by severe proteinuria (≥3.5 gr/d), edema, hypoalbuminemia, and various levels of hyperlipidemia1. There is a clear clinical correlation between proteinuria and subepithelial immune deposition in glomerular diseases that lead to nephrotic syndrome. Immune-mediated proteinuria has thus far been proposed to be induced by two different mechanisms including unspecific accumulation of immunoglobins (Igs) in glomerular capillary (i.e. membranoproliferative glomerulonephritis and systemic lupus nephritis) or binding of specific Igs to podocytes-associated targets leading to disruption and loss of podocytes (i.e. membranous nephropathy)2,3. Podocytes are highly specialized cells with a complex cytoarchitecture. They are composed of tertiary foot processes (FPs), as a major component of the glomerular filtration barrier. An exclusive intracellular junction, known as the slit diaphragm (SD), is responsible for FPs connections, serving as an ultimate barrier to regulate passage of macromolecules from the blood. Alterations of the unique actin-based morphology of FPs are a common feature of kidney disease4. Membranous nephropathy (MN), as one of the most common form of GDs causes NS and subsequently, end-stage renal disease in Caucasian adults, and is a form of immune-mediated glomerular injury characterized by subepithelial deposition of immune complexes, glomerular accumulation of IgG, C3, and C5b-9, and extensive FPs effacement1,5.
In contrast to the regenerative ability of tubular epithelial cells6, replacement of damaged podocytes remains a challenge7. As long as the rate of podocyte loss is limited, recuperation or repair of these cells is possible. Using animal models, it was shown that podocytes depletion of up to 20% can be compensated, most likely through induction of hypertrophy in the adjacent podocytes8. By contrast, a 20–40% loss of the podocytes can cause a scarring response and an over 50% loss of podocytes results in dysfunction of glomeruli filtration. These levels of podocytes depletion are accompanied by corresponding degrees of proteinuria due to the increased proportion of the involved glomeruli and remarkable reductions in renal clearance, as seen in immune-mediated NS9,10,11. Currently, therapeutic protocols for MN are often non-specific12 and rely on suppression of the immune system13,14.
According to recent reports, stem cell-based therapy could potentially be a novel therapeutic approach for chronic kidney diseases (CKD)15,16,17,18. Hence, there are reports on human/mouse iPSCs differentiation into podocytes19,20,21,22,23,24 and use of these cells in vitro23,25 or in vivo26. In addition, a recent study reported the beneficial effects of multilineage-differentiating stress-enduring (Muse) cells in an animal model of focal segmental glomerular sclerosis27. However, the ability of transplanted iPSC-podocytes to restore kidney function and structure in animal models of immune-mediated NS, remains to be studied.
In this study, following anti-podocyte antibody (APA) production, we generated a model of APA-induced heavy proteinuria that resembled human MN and was characterized by the presence of subepithelial immune deposits and podocytes loss. Thereafter, iPSCs from a mouse with proteinuria, were differentiated into podocytes that showed protein marker localization and functional characteristics of podocytes. The data revealed that iPSC-podocyte transplantation (PT) decreased proteinuria and improved histopathological features possibly through replacing lost podocytes.
Results
Generation, purification and characterization of anti-podocyte antibody (APA)
In this experiment, rabbits were immunized with a whole podocyte preparation. Following removal of the blood clot, rabbit anti-podocyte serum was collected, concentrated and complement-inactivated. Then, IgGs were isolated from the serum samples (Supplementary Fig. S1A).
SDS-PAGE analysis of the rabbit anti-mouse IgG showed 2 distinct bands with molecular weights of ~50 and ~25 kDa, indicative of rabbit IgG heavy and light chains, respectively (Supplementary Fig. S1B). Indirect ELISA titration of anti-podocyte IgG showed robust immunoreactivity of the antibody against the differentiated immortalized podocytes, which confirmed its functionality after purification (Supplementary Fig. S1C). Subsequently, immunofluorescence staining revealed specific surface and perinuclear cytoplasmic binding of the purified antibody to podocytes compared to the control (Supplementary Fig. S1D,E). In contrast, no binding in mesangial cells after incubation with APA or preimmune antibody was observed (PI; Supplementary Fig. S1F,G). Flow cytometric analysis results indicated that APA was bound to approximately 95% of the podocyte population (Supplementary Fig. S1H) with no remarkable interactions for APA in mesangial cells (Supplementary Fig. S1I) nor for PI in podocytes and mesangial cells (Supplementary Fig. S1K,L). In addition, no reaction to the isotopic control was observed in the podocyte and mesangial cells (Supplementary Fig. S1J,M). Specific fluorescence could be detected with APA, even at 1:1000 dilution. According to the Bradford assay, the concentration of purified IgG was 7.5 mg/ml.
Generation and characterization of iPSCs from a mouse model of membranous nephropathy
Resemblance of the representative tail-tip fibroblast (TTFs; Supplementary Fig. S2A)- derived iPSCs to generally approved ESC lines, was verified in terms of morphology (Supplementary Fig. S2B); karyotype analysis (Supplementary Fig. S2C); teratoma formation (Supplementary Fig. S2D); and the presence of cells and structures presenting the 3 germ layers within the teratoma (Supplementary Fig. S2E–G); embryoid body (EB) formation (Supplementary Fig. S2H); and alkaline phosphatase expression (Supplementary Fig. S2I). Observations by fluorescence and immunofluorescence microscopy also confirmed the appropriate localization of green fluorescent protein (GFP) in the iPSCs (Supplementary Fig. S2J) and the presence of 4 pluripotency markers (Supplementary Fig. S2K–N) following long-term culture (passages 30–35), respectively.
Differentiation and characterization of podocytes from iPSCs
Figure 1A depicts the protocol we used for differentiation of mouse iPSCs. First, GFP+ iPSC differentiation into nephrogenic intermediate mesoderm (NIM) was induced through formation of EBs (Supplementary Fig. S3A,B,I,J) followed by a culture of EBs. Previous studies that investigated renal differentiation of pluripotent cells relied on Osr1, Pax2, Lhx1, Wt1, Eya1, and Sall1 as definitive markers for NIM formation22,28,29,30,31. According to this evidence, we analyzed their expressions at gene or protein levels. Immunofluorescence staining and quantitative reverse transcription polymerase chain reaction (qRT-PCR) analysis of NIM cells (Supplementary Fig. S3C) showed the expression of Osr1, a key upstream molecule in renal development, and Pax2 and Sall132,33 at the protein levels (Fig. 1B). These cells also expressed Lhx1, Eya1, and Wt1 at the transcriptional levels. Conversely, we observed downregulation of the pluripotency marker Oct4 that occurred from the undifferentiated state to day 8 of differentiation (Fig. 1C). Following culture of NIM cells in basal medium that contained 15 ng/ml BMP7, 1 U/ml LIF, and 150 ng/ml glial cell line-derived neurotrophic factor (GDNF), we observed that the transcription levels of NPC marker genes Six2, Hoxd11, Cited1, Sall1, Eya1, Pax2, and Wt134, up-regulated after day 3 of treatment (Fig. 1D). Key markers of NPCs namely, Six2, Pax2, and Wt1, were detected in iPSC-derived NPCs by immunostaining (Fig. 1E). The proportion of cells that expressed Wt1 and Pax2 increased on day 15 of induction together with expression of podocin as a podocyte marker (Fig. 1F) that represented podocyte progenitors35. The transcription levels of other podocyte marker genes such as Synpo, Nphs1, Cd2ap, and Pdxl, also up-regulated at the same time (Fig. 1G). Interestingly, transcription levels of Nphs119 and Pdxl36 were comparable to those observed for iPSCs.
Generation and characterization of podocytes from induced pluripotent stem cells (iPSCs). (A) Experimental design and optimization of induced pluripotent stem cell (iPSCs) differentiation into podocytes. (B) Immunostaining for nephrogenic intermediate mesoderm (NIM) markers Osr1, Pax2 and Sall1 on day 8. Quantitative RT-PCR analyses of marker gene expression for (C) NIM and (D) NPC cells differentiated from iPSCs on days 8 and 12, respectively. Immunofluorescence analysis of (E) NPC and (F) podocyte progenitor markers. (G) Gene expression analysis confirmed the commitment to the podocyte fate by the increase in podocyte markers. (H) Immunofluorescence analysis for the podocyte marker proteins podocin, podocalyxin, synaptopodin, Wt1, and nephrin displayed a final induction towards green fluorescent protein (GFP)+ mature podocyte cells at passage 6. We also observed the presence of highly organized actin fibers within the podocyte cytoplasm. Immunostaining of iPSC-podocytes with the produced anti-podocyte antibody (APA) showed high immunoreactivity with these cells. (I) Scanning electron microscopy of iPSC-podocytes demonstrated a main cell body and (J) tight junction-like structures that were connected to the adjacent cells (arrows). (K) Cytoplasmic projections that extended from the cell body (arrows) and (L) tertiary projections at the end of processes of the cytoplasmic projections (arrows). (M) Doubling time graph for proliferative differentiated podocytes from iPSCs. (N) Quantitative RT-PCR analyses showed decreased expression levels of Pax2 and increased expression levels for Wt1, Synpo, Nphs2, Nphs1, and Pdxl with increasing culture time. (O) Flow cytometry for podocin in iPSC-podocytes on day 22. Samples treated only with secondary antibodies were used as controls (red). Relative gene expression was normalized against GAPDH. The fold-change values are represented by mean ± SEM (n = 3). Scale bars: B, E, F, and H: 100 µm.
Overall, the cell progeny consisted of uniformly unspecialized and immature criteria with a large, rounded, and often binucleated phenotype (Supplementary Fig. S3D). Most cells differentiated into stretched or multi-angled cells on day 15 (Supplementary Fig. S3E,K). Following cell culture in VRAD + dexamethasone, the proliferative cells were sub-passaged and cultured in Roswell Park Memorial Institute (RPMI)−1640 medium where they developed into large cells that had a typical arborized pattern of foot process extensions (Supplementary Fig. S3F, G,L). The morphology of the latter cells was comparable to immortalized mouse podocytes incubated under non-permissive conditions that displayed characteristics of mature podocytes (Supplementary Fig. S3H).
As shown in Fig. 1H, immunostaining of the iPSC-podocytes showed that podocin, podocalyxin, synaptopodin, and nephrin proteins were localized within the cytoplasm of the cell body, the extensions, or the filamentous arrangement of the iPSC-podocytes. We performed phalloidin staining for filamentous actin (F-actin). F-actin is a filamentous protein that forms the contractile cytoskeleton which is considered to be a key component of podocytes and is necessary for proper glomerular filtration. The results showed the presence of highly organized actin fibers within the podocyte cytoplasm. Despite the expression of both Pax2 and Wt1 in the progenitors, only Wt1 was expressed in sub-passaged podocytes at the protein level. The iPSC-podocytes were also validated by immunostaining using previously generated APA. GFP was detected mainly in the nuclei of the majority of cells because we did not attach any localization signal to GFP when generating GFP+ iPS cells.
Analysis of scanning electron microscopy images showed that iPSC-podocyte had a typical arborized phenotype that consisted of a main cell body with elongated processes which extended to the periphery of the cells (Fig. 1I). There were tight junction-like structures between adjacent cells (Fig. 1J) and secondary as well as tertiary cytoplasmic processes that were projected from the cell bodies (Fig. 1K,L).
Although the iPSC-podocytes could proliferate, we observed growth arrest during passage 6, which confirmed that these podocytes behaved like mature podocytes at this stage (Fig. 1M). qRT-PCR analysis of mRNA expression showed up-regulation of Wt1, Synpo, Nphs2, Nphs1, and Pdxl with increased culture time or passage number. On the other hand, the expression levels of Pax2 decreased (Fig. 1N).
Flow cytometry analysis for podocin revealed an average of 80% efficiency for this differentiation protocol (Fig. 1O).
Functional traits of iPSC-podocytes
Podocytes and their cytoplasmic extensions develop an actin-based contractile system that contracts in response to insulin37 and angiotensin II (AII)19,22. We used immunofluorescence and phase-contrast microscopy to film a time-lapse recording of the dynamic changes in cell morphology. Our data showed that addition of 100 nM of insulin and 500 nM of AII induced contractions in the iPSC-podocyte cell body and shortened cytoplasmic processes (Supplementary Fig. S4A and Movie S1). A permeability assay was performed to assess the endocytic uptake of albumin as further evidence for the functional characteristics of the iPSC-podocytes22,38. Fluorescence microscopy observation of the Texas Red-labelled albumin showed accumulation of vesicles within the cytoplasm near the perinuclear region (Supplementary Fig. S4B).
Therapeutic effect of iPSC-Podocytes on renal function in mice with anti-podocyte antibody (APA) induced proteinuria
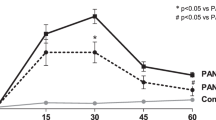
A preliminary experiment of the administered doses showed that APA 2.8 mg/mouse results in initial proteinuria on day 5 that increased to maximum values on days 10–15. Despite a slight reduction within the next 20 days, the proteinuria remained stable until day 60. In addition, albumin content was quantified and corrected for urine creatinine. The urine albumin/creatinine ratio significantly increased to a maximum value on day 15. The control groups consisted of non-treated (NT) mice, whereas the PI groups consisted of mice that received 2.8 mg/mouse of normal rabbit IgG. There was no significant difference in renal functional between the control and PI-treated groups (Fig. 2B–J). Therefore, we used the PI groups as control groups for statistical analyses.
Analysis of serum and urine indices in anti-podocyte antibody (APA) treated and iPSC-podocyte transplanted mice. (A) Timeline of pre-immunization and antibody infusion in mice. Asterisks and hashtags indicate days on which specimens for urine, serum, and histology were obtained. (B–J) Quantification of Upro, Ualb/crea ratio, Stpro, Salb, BUN, Stg, Scho, Uur, and Scr in non-treated (●, NT), preimmune (■, PI), anti-podocyte nephropathy + phosphate-buffered saline (▲, APN + PBS), and APN + podocyte transplantation (▼, APN + PT) mice groups (n = 5) on the indicated days. (K) Serum third complement component (C3) levels in PI and anti-podocyte antibody (APA) treated mice on days 10 and 15 (n = 3). (L) Protein staining of SDS-PAGE gel loaded with 2.5 µl of urine samples collected on the indicated days in the PI, APN + PBS, and APN + PT groups. (M) Left panel: Western blots of urine from day10 probed for mouse IgG (IgG), albumin (alb), podocin (pod), and podocalyxin (pdx). Right panel: Western blots of urine probed for pdx and green fluorescent protein (GFP), 25 days after cell transplantation. The grouping of blots was cropped from different parts of one gel and exposures are made explicit. Values are expressed as mean ± SEM. PI vs. APN + PBS groups: a: p < 0.05, b: p < 0.01, and c: p < 0.001. APN + PBS vs. APN + PT groups: A’: p < 0.05, B’: p < 0.01, and C’: p < 0.001.
Evaluation of complementary system interference revealed no significant difference in serum levels of third complement component (C3) on days 10 and 15 compared to the PI group (Fig. 2K). Immunocytochemistry analysis of the cultured podocytes showed no evidence of any immunoreactivity with serum from APA-treated mice on day 10.
Surprisingly, 10 days after podocyte transplantation (PT), proteinuria significantly decreased in the cell transplanted anti-podocyte nephropathy induced (APN + PT) group (0.393 ± 0.07 mg/dl) compared to the PBS treated anti-podocyte nephropathy induced (APN + PBS) group (0.95 ± 0.16 mg/dl). The urine albumin/creatinine ratio also significantly decreased in the APN + PT group (1447.81 ± 231.07 µg/mg) compared to the APN + PBS group (2571 ± 347.78 µg/mg), 25 days after PT. No significant changes observed at these levels until day 50 after transplantation (Fig. 2B,C).
We observed significantly higher serum total protein and albumin levels compared to the APN + PBS group after transplantation of the cells (Fig. 2D,E). There were decreased levels of serum urea nitrogen, triglycerides, and cholesterol by the time in the podocyte-transplanted groups (Fig. 2F–H). In contrast, no significant change was observed in urea content of the urine samples during the entire experiment in any of these groups (Fig. 2I). Of note, the increased serum creatinine levels did not change up to day 50, while serum creatinine decreased on day 60 in the podocyte-transplanted groups (Fig. 2J).
We also evaluated proteinuria by SDS-PAGE of the urine samples from PI, APN + PBS, and APN + PT groups. The urine protein content decreased in the APN + PT group compared to the nephrotic mice from the APN + PBS group (Fig. 2L). Western blot analysis of proteinuria in mouse urine showed the presence of IgG, albumin, and podocyte-specific protein content such as podocin and podocalyxin, which indicated podocyte damage within the glomeruli due to APA-induced proteinuria (Fig. 2M). Western blot analysis of the urine sample from the cell-transplanted mice also showed podocalyxin and a weak band of GFP (Fig. 2M) which indicated possible transplanted GFP+ podocyte damage or death.
Renal histopathologic changes in proteinuria induced and cell-transplanted mice
Histological analyses of mice nephrotic injury on day 10 showed increased mesangial matrix associated with some degrees of crescent and diffuse mesangial sclerosis (Fig. 3A), decreased Wt1+ podocyte numbers (Fig. 3B,E), and increased glomerular section area (Fig. 3F), compared to the NT and PI treated mice. We observed no remarkable pathological changes in the distal and proximal tubules. In addition, no GFP+ cell was observed in the lung and liver, 40- and 50-day post-transplantation.
Altered histopathology of membranous nephropathy (MN) obtained from 100 glomeruli per group (n = 5) with similar staining patterns on day 10. (A) Hematoxylin and eosin (H&E), Masson’s trichrome (MT), and periodic acid-Schiff (PAS) stained kidney sections from non-treated (NT), preimmune antibody (PI), and anti-podocyte antibody (APA) treated mice showed increased mesangial matrix and diffuse mesangial sclerosis with an occasional tendency for glomerular crescents (asterisks). (B) Representative pictures for immunohistochemical (IHC) staining of Wt1 as a podocyte marker in glomeruli of the 3 mice groups. (C) Transmission electron microscopy (TEM) revealed podocyte vacuolization with blebbing, foot process effacement, and detachment from the GBM in APA-treated mice (arrows). (D) Electron microscopy showed subepithelial electron dense deposits. Immunofluorescence study results showed the presence of APA, coarse granular deposits of IgG and C3 together whit C3b. (E) Quantitation of the numbers of Wt1-positive podocytes in the glomeruli of the 3 mice groups. (F) Quantitative analysis of glomerular section areas of the 3 mice groups. All values are presented as mean ± SEM. Differences were determined by ANOVA and a subsequent Tukey test. p < 0.05 was considered statistically significant. **p < 0.01, ***p < 0.001, and ns: Not significant. Scale bars in A and B: 100 µm.
Transmission electron microscopy (TEM) analysis of tissues from mice with proteinuria showed evidence of podocyte vacuolization, blebs, foot process effacement, and detachment from the glomerular basement membrane (GBM) compared with the control groups (Fig. 3C). TEM also revealed subepithelial electron dense deposits. Immunofluorescence exhibited the presence of APA, coarse granular deposits of IgG, C3, and C3b into glomerular tuft (Fig. 3D), whereas control mice did not show IgG reactivity and C3 deposition (Supplementary Fig. S5). In contrast, C1q and C4b, as the complement components, were not detected within the glomeruli.
We sought to determine if iPSC-PT has a beneficial effect on regeneration or repair after APN. Since the earliest time point at which a significant decrease in proteinuria was observed, was day 20, the mice were sacrificed on days 20, 50, and 60 and we conducted histological investigations of their renal tissues. Light microscopy assessment showed no significant pathological changes in the proximal and distal tubules throughout the observation period. The injected cells were mainly located in the cortex; however, these cells were also scattered throughout the medulla sections of the transplanted mice and occasionally in the cortical tubules (Supplementary Fig. S6). Ten days after the iPSC-PT, there were significant changes in the glomeruli that remained for an additional 40 days. We observed a significant improvement in glomerular pathologies in the podocyte-transplanted mice (Figs 4 and 5A,B). These beneficial effects were associated with a significant decrease in glomerular section area (µ2) in the cell-treated groups (similar to the PI-treated mice) compared to the APN + PBS groups throughout the experimental period. The glomerular section area on day 50 in these groups was 968.7 ± 36 µ2 for APN + PT, 1238.35 ± 39 µ2 for APN + PBS, and 1049 ± 33.2 µ2 for PI. On day 60, it was 1052.2 ± 42.1 µ2 for APN + PT, 1195 ± 38.8 µ2 for APN + PBS, and 1007.5 ± 33.2 µ2 for PI as seen in Fig. 5C. Immunohistological (IHC) studies of the kidney sections demonstrated that the number of Wt1+ podocytes decreased by approximately 50% in APA (13.2 ± 0.4) compared to PI treated (25.3 ± 0.7) mice on day 10 (Fig. 3E). The podocyte population was 17 ± 0.8 (APN + PBS) compared to 24.8 ± 0.9 (PI) on day 60 (Fig. 5D). It seems that almost 4 podocytes were ineffectively regenerated by possible renal progenitor cells until the end of the experiment. Interestingly, there was a significant increase in the glomerular podocyte population in the APN + PT groups compared to the APN + PBS groups throughout the experimental period (Supplementary Table S4).
Histopathology section of kidney specimens obtained from anti-podocyte nephropathy + phosphate-buffered saline (APN + PBS), preimmune antibody (PI), and podocyte transplantation (APN + PT) groups on days 20, 50, and 60. Representative images show hematoxylin and eosin (H&E), Masson’s trichrome (MT), and periodic acid-Schiff (PAS) staining of the kidney sections. The arrows indicate increased mesangial matrix, diffuse mesangial sclerosis with some degrees of crescent formation in the anti-podocyte nephropathy + phosphate-buffered saline (APN + PBS) groups (vehicle) compared to the preimmune antibody (PI) groups (control groups). In contrast, the representative images show significant improvement against damaged glomeruli of the cell-transplanted groups (APN + PT) compared to vehicle groups on the respective days. Scale bars: 100 µm.
Attenuation of podocyte lesion-related histological damage after induced pluripotent stem cell-podocyte transplantation (iPSC-PT) into mice with membranous nephropathy. (A,B) Percentages of glomerular pathologies; (C) glomerular section areas; (D) the numbers of Wt1-positive cells in the glomeruli of the 3 groups: preimmune antibody (PI), anti-podocyte nephropathy + phosphate-buffered saline (APN + PBS), and podocyte transplantation (APN + PT) on the indicated days.
The Wt1+ podocyte numbers on day 20 were 24.1 ± 0.9 (APN + PT), 14.4 ± 0.8 (APN + PBS), and 25.4 ± 0.7 (PI). On day 50, these values were 21.5 ± 0.8 (APN + PT), 16.1 ± 0.7 (APN + PBS), and 23.7 ± 0.8 (PI). On day 60, these values were 22.5 ± 0.9 (APN + PT), 17 ± 0.8 (APN + PBS), and 24.8 ± 0.8 (PI) as seen in Fig. 5D. However, in the cell-transplanted mice, the highest number of GFP+ iPSC-podocytes localized in the glomeruli 10 days after transplantation (9.8 ± 0.5 GFP+ podocyte/glo. sec. area) followed by 8.2 ± 0.4 GFP+ podocyte/glo. sec. area (day 40 of PT), and 7.1 ± 0.3 GFP+ podocyte/glo. sec. area (day 50 of PT; Fig. 6A,B). Finally, immunogold staining confirmed the incorporation of GFP+ podocytes in the glomeruli with apicobasal polarity and formation of SD-like structures between the FPs of newly integrated podocytes (Fig. 6C).
Qualitative and quantitative analysis of localization of transplanted podocytes. (A) Immunohistochemical (IHC) staining for localization of green fluorescent protein (GFP)+ positive transplanted induced pluripotent stem cell (iPSC)-podocytes in glomeruli 10, 40, and 50 days after cell transplantation. The maximum glomerular localization was observed 10 days after transplantation and continued up to day 50. In addition, the number of extraglomerular transplanted podocytes decreased over time. Scale bars: 100 µm. (B) Quantitation of the numbers of GFP+ iPSC-podocytes localized in the glomeruli. (C) Representative image of immunogold labelling confirmed the incorporation of GFP+ podocytes in glomeruli with apicobasal polarity and formation of slit diaphragm-like structures (arrows) between the foot processes of newly integrated podocytes, 10 days after transplantation. Scale bars: left panel: 5 µm, right panels: 500 nm. Data obtained from 100 glomeruli per group (n = 5 per group). All values are presented as mean ± SEM. Differences were determined by ANOVA and a subsequent Tukey test with p < 0.05 considered statistically significant. *p < 0.05; **p < 0.01; ***p < 0.001; and ns: Not significant.
Discussion
Recent experiments have demonstrated that cell-based therapy as a novel strategy is potentially a promising approach for treatment of the kidney diseases or slowing its progression. Thus, in this field, cell therapy currently focuses on preclinical studies. Preclinical investigations have revealed beneficial effects of various stem cells and stem cell-derived cells in acute/chronic kidney injury models, suggesting a renal regenerative effect for the cell-based therapies39. Among various candidates, iPSCs have shown promising therapeutic potential for kidney disorders40,41,42. This is supported by several studies demonstrating the differentiation of iPSCs into renal lineage20,34,43,44 and organoids45,46 as well as their capabilities for in-vivo transplantation47,48 and generating complex kidney structures49,50.
There is a growing interest in stem cells’ differentiation into defined renal cells such as tubular31,51 and podocyte cells20,22,24,34,52. Despite reports on the therapeutic effects of iPSC-derived podocytes in experimental models26,53, no investigation has evaluated the potential therapeutic effects of iPSC-podocytes in an animal model of immune-mediated podocyte injury.
To this end, we generated an experimental model of MN5,54 by injection of rabbit polyclonal APA into mice which led to direct antibody-mediated damage of podocytes55,56. This model setting exhibited proteinuria associated with GBM disruption, podocyte FPs effacement, subepithelial electron dense deposits that quite closely recapitulates the morphologic hallmarks of human MN. While our serum analysis showed no significant difference in serum levels of C3 our stainings showed deposition of IgG, C3, and C3b on glomeruli together with rabbit polyclonal APA. It is assumed that based on our negative results for C1q and C4b, glomerular injury could possibly be mediated by other mechanisms than complement or at least not via the classical pathway55,56.
Thereafter, we developed a 3-stage protocol to obtain functional podocytes from proteinuria-induced mouse iPSCs which were evaluated with respect to constitutive and induced expression of podocyte markers. We initially used a previously reported protocol29 optimized for inducing the differentiation of NIM cells from mouse iPSCs. This protocol used a combination of activin A, CHIR99021 (glycogen synthase kinase 3β inhibitor), and TTNPB (pan retinoic acid receptor agonist) followed by combined treatment with bone morphogenetic protein (BMP)7, recombinant mouse leukemia inhibitory factor (mLIF), and TTNPB. The induced NIM cells expressed Osr1, Pax2, and Sall1 in conjunction with other NIM markers, Lhx1, Eya1, and Wt157. NIM cells were subsequently differentiated into NPCs by treatment with BMP7, mLIF, and GDNF that expressed the specific transcription factors Six2, Hoxd11, Cited1, Pax2, and Wt134. The podocyte cells had typical morphologic features; transcriptome expressions of Synpo, Nphs1, Pdxl, Nphs2, Wt1, and Pax2; and proteins (nephrin, synaptopodin, podocin, podocalyxin, and Wt1) – all essential, well-described markers of podocytes58 as well as actin cytoskeleton, as an important part of the podocyte-GBM interaction59. They also lost proliferative capacity at passage 6 exhibiting key podocyte phenotypes such as actin reorganization upon insulin or AII stimulation and albumin uptake. The protocol established in this study to differentiate iPSCs into podocytes was approximately 80% efficient in the presence of podocin as a podocyte marker protein.
Next, iPSC-derived cell suspension was slowly injected into different sites of the renal cortex parenchyma of APN-induced mice and relative improvements in renal function and critical amelioration of glomerular defects were observed. The immunohistochemical and immunogold electron microscopy analyses showed integration of GFP+ podocytes in glomeruli with apicobasal polarity, and formation of FPs and SD-like structures suggesting their contribution to reconstruction of the injured filtration barrier. According to our results, it is tempting to speculate that injured glomeruli could possibly provide a molecular recognition sink for transplanted iPSC-podocytes to migrate and incorporate into the injured glomeruli60. This result is also consistent with previous reports showing the integration of podocytes with glomeruli, indicating their capability in regeneration of injured renal structure and function19,26.
Although injected cells were mainly distributed in the cortex, they exhibited a scattered distribution pattern in the medulla sections and were occasionally found in the cortical tubules; however, they were not observed in the lung and liver, as the main organs of the vascular system. This finding might be attributed to the existence of differentiated tubular cells in injected cell population and also dedifferentiation of not-integrated iPSC-podocytes into tubular and/or other cells leading to their distribution in non-glomerular areas. We did not observe remarkable pathological changes in the examined areas; however, dedifferentiation of transplanted iPSC-podocytes and characterization of iPSC-non-podocyte cells should be investigated in further studies to explain the present findings.
On the other hand, we observed the presence of podocalyxin and GFP in the urine of mice during the post-transplantation period. This finding indicated possible damage or death of the transplanted GFP+ podocytes that led to reductions in the number of transplanted cells over time. This observation could be attributed to the rigors such as mechanical stress during implantation, extracellular matrix loss upon delivery, nutrient and oxygen deprivation at the recipient site, and host inflammatory response which are detrimental factors that limit long-term survival of transplanted cells61,62,63. Of note, the majority of regenerated podocytes in the treated APN mice, was originated from the transplanted cells, which suggested that purified iPSC-podocytes transplanted by an improved approach, might enhance the therapeutic efficacy of transplanted cells. The remainder of the regenerated podocytes might be induced by differentiation of the putative progenitor cells derived from the glomerular parietal epithelium of Bowman’s capsule64, which likely occurred via triggering Notch65 and Wnt-β-catenin pathways66. Therefore, accumulating evidence points to the attenuation effect of transplanted cells on proteinuria. We propose this effect is related to integration and replacement of transplanted cells and to some extent, the recruitment of intrinsic glomerular progenitors in responses to damages to podocyte pathways. Further work is required for characterization of nonintegrated cells and development of strategies that aim at improvement of viable cell engraftment and survival. Finally, it should be noted that generalization of the results of this study to human disease requires further studies to solve above mentioned limitations.
Conclusions
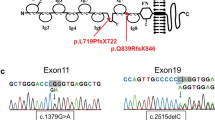
We demonstrated that the transplanted iPSC-podocytes could restore injured kidney function and improve pathological indices in an experimental model of MN. These findings suggested that autologous and patient-specific iPSC-podocytes (potentially with correction of defective genes) could be a potential cellular resource for stem cell-based therapy for MN and hereditary forms of CKD. Finally, it could be an initial pace to navigate a therapeutic approach for individuals who suffer from CKD due to loss of podocytes.
Methods
Animal procedures and cell culture
All animal care, including experimental, surgical, and postoperative euthanasia procedures were performed in strict accordance with the ethical principles of the NIH Guide for the Care and Use of Laboratory Animals and approval by the Institutional Review Board and Ethical Committee at Royan Institute (No. EC.89.1061). Supplementary information provides more details on animal procedures, and podocyte and mesangial cell line culture protocol.
Anti-podocyte antibody (APA) production, purification, and characterization
Rabbit polyclonal antibody against murine podocytes was generated, purified, and characterized as previously described with few modifications (Supplementary information).
Generation of a mouse model of membranous nephropathy
This procedure was carried out as previously described with few modifications. Briefly, the animals received intravenous (IV) administration of APA 5 days after subcutaneous pre-immunization. Then, urine, serum, and tissue samples were collected (Supplementary information).
iPSCs generation and characterization
iPSCs were derived from induced APN mouse TTFs by retroviral transfection of Oct4, Sox2, Klf4, and c-Myc (Addgene) as previously described (Supplementary information).
iPSCs differentiation into podocytes
We converted the iPSCs into podocytes via a series of modified differentiation procedures to obtain stage-specific cell types of NIM, NPC, podocyte progenitors, and podocytes (Supplementary information).
Cell proliferation assay
On day 22 of the differentiation protocol, iPSC-podocytes were seeded in 4-well plates at approximately 40% confluency. We determined the proliferation rate, expressed as doubling times, by fitting the % phase object confluence data points between day 0 to the day when cells reached 80% confluency for the next subcultures. The subcultures were continued until the cells exhibited a growth arrest. Undifferentiated E11 cells were cultured as a control group.
Functional assays
Functional assays for iPSC-podocytes included the reorganization of F-actin cytoskeleton and contractile response to the addition of insulin (100 nM) and AII (500 nM), and the endocytosis of albumin (Supplementary information).
Cell transplantation
We transplanted passage-6 iPSC-cells into the renal cortex parenchyma by a micropipette connected to a microinjector, 10 days after antibody treatment (Supplementary Fig. S7). The control group received PBS injections (Supplementary information).
Evaluation of urine, serum, and histopathological indices
Supplementary information provides details on urine, serum, and histopathologic analyses and quantification of podocyte numbers.
Statistical analysis
Values represent mean ± standard error of mean (SEM). Analysis was performed using GraphPad Prism 6.01. Differences among the experimental groups were tested by means of two-way analysis of variance with the Tukey multiple comparison test. The independent sample student’s t-tests were performed to identify significant differences in serum levels of the C3 value of the control and day 10 or 15, as well as differences in podocyte numbers at the indicated times. Statistical significance was set at p < 0.05.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Change history
05 July 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41598-021-93174-z
References
Lai, W. L. et al. Membranous nephropathy: a review on the pathogenesis, diagnosis, and treatment. J. Formos. Med. Assoc. 114, 102–111 (2015).
Asanuma, K. & Mundel, P. The role of podocytes in glomerular pathobiology. Clin. Exp. Nephrol. 7, 255–259, https://doi.org/10.1007/s10157-003-0259-6 (2003).
Meliambro, K., He, J. C. & Campbell, K. N. The podocyte as a therapeutic target in proteinuric kidney disease. Journal of Nephrology & Therapeutics 2013 (2013).
Martin, C. E. & Jones, N. Nephrin signaling in the podocyte: an updated view of signal regulation at the slit diaphragm and beyond. Front. Endocrinol. (Lausanne) 9, 302 (2018).
Luo, W. et al. Alternative pathway is essential for glomerular complement activation and proteinuria in a mouse model of membranous nephropathy. Front. Immunol. 9, 1433 (2018).
Humphreys, B. D. & Bonventre, J. V. The contribution of adult stem cells to renal repair. Nephrol. Ther. 3, 3–10 (2007).
Hagen, M. et al. Cell cycle re-entry sensitizes podocytes to injury induced death. Cell Cycle 15, 1929–1937 (2016).
Wiggins, J. E. et al. Podocyte hypertrophy,“adaptation,” and “decompensation” associated with glomerular enlargement and glomerulosclerosis in the aging rat: prevention by calorie restriction. J. Am. Soc. Nephrol. 16, 2953–2966 (2005).
Wiggins, R. C. The spectrum of podocytopathies: a unifying view of glomerular diseases. Kidney Int. 71, 1205–1214, https://doi.org/10.1038/sj.ki.5002222 (2007).
Cook, H. T. Focal segmental glomerulosclerosis in IgA nephropathy: a result of primary podocyte injury? Kidney Int. 79, 581–583, https://doi.org/10.1038/ki.2010.521 (2011).
Kerjaschki, D. Pathomechanisms and molecular basis of membranous glomerulopathy. The Lancet 364, 1194–1196 (2004).
El-Husseini, A. et al. Idiopathic Membranous Nephropathy: Diagnostic and Therapeutic Challenges. Am. J. Nephrol. 43, 65–70 (2016).
Holdsworth, S. R., Gan, P.-Y. & Kitching, A. R. Biologics for the treatment of autoimmune renal diseases. Nature Reviews Nephrology (2016).
Debiec, H. et al. Allo-immune membranous nephropathy and recombinant aryl sulfatase replacement therapy: a need for tolerance induction therapy. J. Am. Soc. Nephrol., ASN. 2013030290 (2013).
Wang, S., Li, Y., Zhao, J., Zhang, J. & Huang, Y. Mesenchymal stem cells ameliorate podocyte injury and proteinuria in a type 1 diabetic nephropathy rat model. Biol. Blood Marrow Transplant. 19, 538–546 (2013).
Papazova, D. A. et al. Cell-based therapies for experimental chronic kidney disease: a systematic review and meta-analysis. Disease Models and Mechanisms 8, 281–293 (2015).
Jiang, Y. et al. Transplantation of human fetal pancreatic progenitor cells ameliorates renal injury in streptozotocin-induced diabetic nephropathy. J. Transl. Med. 15, 147 (2017).
Moschidou, D. et al. Human chorionic stem cells: podocyte differentiation and potential for the treatment of alport syndrome. Stem cells and development 25, 395–404 (2016).
Song, B. et al. The directed differentiation of human iPS cells into kidney podocytes. PLoS One 7, e46453, https://doi.org/10.1371/journal.pone.0046453 (2012).
Morizane, R. & Lam, A. Q. Directed Differentiation of Pluripotent Stem Cells into Kidney. Biomarker insights 10, 147 (2015).
Morizane, R., Monkawa, T. & Itoh, H. Differentiation of murine embryonic stem and induced pluripotent stem cells to renal lineage in vitro. Biochemical and biophysical research communications 390, 1334–1339 (2009).
Ciampi, O. et al. Generation of functional podocytes from human induced pluripotent stem cells. Stem cell research 17, 130–139 (2016).
Musah, S., Dimitrakakis, N., Camacho, D. M., Church, G. M. & Ingber, D. E. Directed differentiation of human induced pluripotent stem cells into mature kidney podocytes and establishment of a Glomerulus Chip. Nat. Protoc. 13, 1662–1685 (2018).
Rauch, C. et al. Differentiation of human iPSCs into functional podocytes. PLoS One 13, e0203869 (2018).
Musah, S. et al. Mature induced-pluripotent-stem-cell-derived human podocytes reconstitute kidney glomerular-capillary-wall function on a chip. Nature Biomedical Engineering 1, 0069 (2017).
Sharmin, S. et al. Human induced pluripotent stem cell–derived podocytes mature into vascularized glomeruli upon experimental transplantation. J. Am. Soc. Nephrol. 27, 1778–1791 (2016).
Uchida, N. et al. Beneficial effects of systemically administered human muse cells in adriamycin nephropathy. Journal of the American Society of Nephrology, ASN. 2016070775 (2017).
Oeda, S. et al. Induction of intermediate mesoderm by retinoic acid receptor signaling from differentiating mouse embryonic stem cells. The International Journal of Developmental Biology 57, 383–389, https://doi.org/10.1387/ijdb.130058ma (2013).
Mae, S. et al. Monitoring and robust induction of nephrogenic intermediate mesoderm from human pluripotent stem cells. Nat Commun 4, 1367, https://doi.org/10.1038/ncomms2378 (2013).
Kumar, N. et al. Generation of an expandable intermediate mesoderm restricted progenitor cell line from human pluripotent stem cells. Elife 4, e08413 (2015).
Lam, A. Q. et al. Rapid and efficient differentiation of human pluripotent stem cells into intermediate mesoderm that forms tubules expressing kidney proximal tubular markers. J. Am. Soc. Nephrol., ASN. 2013080831 (2013).
Mugford, J. W., Sipilä, P., McMahon, J. A. & McMahon, A. P. Osr1 expression demarcates a multi-potent population of intermediate mesoderm that undergoes progressive restriction to an Osr1-dependent nephron progenitor compartment within the mammalian kidney. Dev. Biol. 324, 88–98 (2008).
Dressler, G. R. The cellular basis of kidney development. Annu. Rev. Cell Dev. Biol. 22, 509–529 (2006).
Kang, M. & Han, Y.-M. Differentiation of human pluripotent stem cells into nephron progenitor cells in a serum and feeder free system. PLoS One 9, e94888 (2014).
Lasagni, L. et al. Podocyte regeneration driven by renal progenitors determines glomerular disease remission and can be pharmacologically enhanced. Stem Cell Reports 5, 248–263 (2015).
Tateno, H. et al. Podocalyxin Is a Glycoprotein Ligand of the Human Pluripotent Stem Cell‐Specific Probe rBC2LCN. Stem cells translational medicine 2, 265–273 (2013).
Welsh, G. I. et al. Insulin signaling to the glomerular podocyte is critical for normal kidney function. Cell Metab. 12, 329–340 (2010).
Xinaris, C. et al. Functional human podocytes generated in organoids from amniotic fluid stem cells. J. Am. Soc. Nephrol. 27, 1400–1411 (2016).
Marcheque, J., Bussolati, B., Csete, M. & Perin, L. Concise Reviews: Stem Cells and Kidney Regeneration: An Update. Stem cells translational medicine 8, 82–92 (2019).
Imberti, B. et al. Renal progenitors derived from human iPSCs engraft and restore function in a mouse model of acute kidney injury. Sci. Rep. 5 (2015).
Li, Q. et al. Transplantation of induced pluripotent stem cell-derived renal stem cells improved acute kidney injury. Cell Biosci 5, 45, https://doi.org/10.1186/s13578-015-0040-z (2015).
Toyohara, T. et al. Cell therapy using human induced pluripotent stem cell-derived renal progenitors ameliorates acute kidney injury in mice. Stem Cells Transl Med 4, 980–992 (2015).
Morizane, R., Monkawa, T. & Itoh, H. Differentiation of murine embryonic stem and induced pluripotent stem cells to renal lineage in vitro. Biochem. Biophys. Res. Commun. 390, 1334–1339, https://doi.org/10.1016/j.bbrc.2009.10.148 (2009).
Lam, A. Q., Freedman, B. S. & Bonventre, J. V. Directed differentiation of pluripotent stem cells to kidney cells. Semin. Nephrol. 34, 445–461, https://doi.org/10.1016/j.semnephrol.2014.06.011 (2014).
Morizane, R. et al. Nephron organoids derived from human pluripotent stem cells model kidney development and injury. Nat. Biotechnol. 33, 1193 (2015).
Hiratsuka, K. et al. Induction of human pluripotent stem cells into kidney tissues by synthetic mRNAs encoding transcription factors. Sci. Rep. 9, 913 (2019).
Tajiri, S. et al. Regenerative potential of induced pluripotent stem cells derived from patients undergoing haemodialysis in kidney regeneration. Sci. Rep. 8, 14919 (2018).
van den Berg, C. W. et al. Renal subcapsular transplantation of PSC-derived kidney organoids induces neo-vasculogenesis and significant glomerular and tubular maturation in vivo. Stem Cell Reports 10, 751–765 (2018).
Taguchi, A. et al. Redefining the in vivo origin of metanephric nephron progenitors enables generation of complex kidney structures from pluripotent stem cells. Cell stem cell 14, 53–67 (2014).
Takasato, M. et al. Directing human embryonic stem cell differentiation towards a renal lineage generates a self-organizing kidney. Nat. Cell Biol. 16, 118–126, https://doi.org/10.1038/ncb2894 (2014).
Lazzeri, E. et al. Human urine-derived renal progenitors for personalized modeling of genetic kidney disorders. J. Am. Soc. Nephrol., ASN. 2014010057 (2015).
Qian, T. et al. Directed Differentiation of Human Pluripotent Stem Cells to Podocytes under Defined Conditions. Sci. Rep. 9, 2765 (2019).
Tanigawa, S. et al. Organoids from nephrotic disease-derived iPSCs identify impaired NEPHRIN localization and slit diaphragm formation in kidney podocytes. Stem cell reports 11, 727–740 (2018).
Borza, D.-B., Zhang, J.-J., Beck, L. H. Jr., Meyer-Schwesinger, C. & Luo, W. Mouse models of membranous nephropathy: the road less travelled by. American journal of clinical and experimental immunology 2, 135 (2013).
Meyer, T. N. et al. A new mouse model of immune-mediated podocyte injury. Kidney Int. 72, 841–852, https://doi.org/10.1038/sj.ki.5002450 (2007).
Meyer-Schwesinger, C. et al. Nephrotic syndrome and subepithelial deposits in a mouse model of immune-mediated anti-podocyte glomerulonephritis. J. Immunol. 187, 3218–3229, https://doi.org/10.4049/jimmunol.1003451 (2011).
Kim, D. & Dressler, G. R. Nephrogenic factors promote differentiation of mouse embryonic stem cells into renal epithelia. J. Am. Soc. Nephrol. 16, 3527–3534 (2005).
Shankland, S. J., Pippin, J. W., Reiser, J. & Mundel, P. Podocytes in culture: past, present, and future. Kidney Int. 72, 26–36, 10.1038/sj.ki.5002291 (2007).
Oh, J., Reiser, J. & Mundel, P. Dynamic (re) organization of the podocyte actin cytoskeleton in the nephrotic syndrome. Pediatr. Nephrol. 19, 130–137 (2004).
Sugimoto, H. et al. Bone-marrow-derived stem cells repair basement membrane collagen defects and reverse genetic kidney disease. Proceedings of the National Academy of Sciences 103, 7321–7326 (2006).
Baldari, S. et al. Challenges and Strategies for Improving the Regenerative Effects of Mesenchymal Stromal Cell-Based Therapies. International journal of molecular sciences 18, 2087 (2017).
Trounson, A. & McDonald, C. Stem cell therapies in clinical trials: progress and challenges. Cell stem cell 17, 11–22 (2015).
Copland, I. B. & Galipeau, J. In Semin. Immunopathol. 535 (Springer).
Appel, D. et al. Recruitment of podocytes from glomerular parietal epithelial cells. J. Am. Soc. Nephrol. 20, 333–343 (2009).
Lasagni, L. et al. Notch activation differentially regulates renal progenitors proliferation and differentiation toward the podocyte lineage in glomerular disorders. Stem Cells 28, 1674–1685 (2010).
Shkreli, M. et al. Reversible cell-cycle entry in adult kidney podocytes through regulated control of telomerase and Wnt signaling. Nat. Med. 18, 111–119 (2012).
Acknowledgements
We would like to express our sincere appreciation to Dr. Florian Grahammer for critically reviewing the manuscript and Dr. Mehri Haeili, Dr. Vahdat Ahmadi, Dr. Koorosh Shahpasand, Payam Teheri, Javad Firouzi, Mojgan Khalili Ghara-aghaji, and Zahra Ajdari for their contributions and excellent technical assistance. We are also deeply indebted to Dr. Fatemeh Nili, Dr. Arash Pourgholaminejad, and Najmeh Masoudi for performing the immunohistochemistry for complement products, interpretation of complement staining, and karyotype analysis, respectively. This study was supported by a grant from Royan Institute and the Royan Charity Association for Health Research.
Author information
Authors and Affiliations
Contributions
A.A., R.M., H.B. and N.A. conceived and designed the study and approved the manuscript. A.A. performed experiments and statistical analysis and wrote the manuscript. V.E. performed qRT-PCR and edited the manuscript. F.H. performed western blot and SDS-PAGE experiments. Z.T. produced, characterized, and maintained the GFP+ iPSC culture. S.M.N. analyzed the pathological data. M.H.A.V. performed the cell transplantation and animal surgery. M.A. participated in production of rabbit anti-mouse podocyte antibody. R.R. performed the immunogold electron microscopy. R.S.Y. performed urine analysis.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ahmadi, A., Moghadasali, R., Ezzatizadeh, V. et al. RETRACTED ARTICLE: Transplantation of Mouse Induced Pluripotent Stem Cell-Derived Podocytes in a Mouse Model of Membranous Nephropathy Attenuates Proteinuria. Sci Rep 9, 15467 (2019). https://doi.org/10.1038/s41598-019-51770-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-51770-0
This article is cited by
-
Therapeutic potential of human induced pluripotent stem cells and renal progenitor cells in experimental chronic kidney disease
Stem Cell Research & Therapy (2020)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.