Abstract
The incidence of penile squamous cell carcinoma (PSCC) has increased in developed countries over the past decades owing to increased human papilloma virus (HPV) exposure. Despite successful surgical treatment of locoregional PSCC, effective treatment options for advanced disease are limited. The prognosis of patients with bulky nodal and metastatic PSCC is dismal and new management approaches are urgently needed. Genomic analyses have provided transformative knowledge on the genomic and molecular landscape and tumour microenvironment of PSCC. Around one-quarter of patients with metastatic PSCC have clinically actionable genomic alterations in mechanistic target of rapamycin, DNA repair and receptor tyrosine kinase pathways. These patients might benefit from combined and sequential targeted therapies. HPV vaccination might be another therapeutic option as PSCC is genetically similar to other HPV-driven cancers. In addition, 40–60% of PSCC tumours show strong PDL1 expression, and the frequency of mutational signatures suggestive of immunotherapy resistance is low, pointing to potential utility of immunotherapy for PSCC. Finally, identification of the composition of the penile microbiota and its biological role might lead to new cancer prevention and treatment strategies.
Key points
-
Penile squamous cell carcinoma (PSCC) displays a wide range of therapeutically targetable somatic alterations, and patients with treatment-resistant advanced PSCC might benefit from combined and sequential targeted therapies.
-
PSCC seems to be genetically similar to other human papilloma virus (HPV)-driven cancers and HPV vaccination might be a useful therapeutic option in nearly half of patients with PSCC infected with high-risk HPV.
-
Particular subsets of patients with PSCC might benefit from immunotherapy as some PSCC tumours display strong PDL1 expression and a low frequency of mutational signatures suggestive of immunotherapy resistance.
-
The evaluation of the spatial relationship between cellular and molecular components by multiplex immunofluorescence immunohistochemistry might provide valuable insights into the molecular profile of PSCC.
-
Further research to identify the composition of the penile microbiota and its association with HPV infection and penile cancer oncogenesis might lead to new cancer prevention and treatment strategies for PSCC.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Hansen, B. T., Orumaa, M., Lie, A. K., Brennhovd, B. & Nygard, M. Trends in incidence, mortality and survival of penile squamous cell carcinoma in Norway 1956–2015. Int. J. Cancer 142, 1586–1593 (2018).
Pham, M. N. et al. Contemporary survival trends in penile cancer: results from the National Cancer Database. Urol. Oncol. 35, 674.e1–674.e9 (2017).
Arya, M. et al. Long-term trends in incidence, survival and mortality of primary penile cancer in England. Cancer Causes Control 24, 2169–2176 (2013).
Ficarra, V., Akduman, B., Bouchot, O., Palou, J. & Tobias-Machado, M. Prognostic factors in penile cancer. Urology 76, S66–S73 (2010).
Veeratterapillay, R., Teo, L., Asterling, S. & Greene, D. Oncologic outcomes of penile cancer treatment at a UK supraregional center. Urology 85, 1097–1103 (2015).
Horenblas, S. Lymphadenectomy for squamous cell carcinoma of the penis. Part 2: the role and technique of lymph node dissection. BJU Int. 88, 473–483 (2001).
Pagliaro, L. C. et al. Neoadjuvant paclitaxel, ifosfamide, and cisplatin chemotherapy for metastatic penile cancer: a phase II study. J. Clin. Oncol. 28, 3851–3857 (2010).
Nicholson, S. et al. Phase II trial of docetaxel, cisplatin and 5FU chemotherapy in locally advanced and metastatic penis cancer (CRUK/09/001). Br. J. Cancer 109, 2554–2559 (2013).
Haas, G. P. et al. Cisplatin, methotrexate and bleomycin for the treatment of carcinoma of the penis: a Southwest Oncology Group study. J. Urol. 161, 1823–1825 (1999).
Carthon, B. C., Ng, C. S., Pettaway, C. A. & Pagliaro, L. C. Epidermal growth factor receptor-targeted therapy in locally advanced or metastatic squamous cell carcinoma of the penis. BJU Int. 113, 871–877 (2014).
Necchi, A. et al. Panitumumab treatment for advanced penile squamous cell carcinoma when surgery and chemotherapy have failed. Clin. Genitourin. Cancer 14, 231–236 (2016).
Hakenberg, O. W. et al. The diagnosis and treatment of penile cancer. Dtsch. Arztebl. Int. 115, 646–652 (2018).
Djajadiningrat, R. S., Bergman, A. M., van Werkhoven, E., Vegt, E. & Horenblas, S. Neoadjuvant taxane-based combination chemotherapy in patients with advanced penile cancer. Clin. Genitourin. Cancer 13, 44–49 (2015).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02305654 (2019).
Canter, D. J. et al. The International Penile Advanced Cancer Trial (InPACT): rationale and current status. Eur. Urol. Focus. 5, 706–709 (2019).
Hernandez, B. Y. et al. Burden of invasive squamous cell carcinoma of the penis in the United States, 1998–2003. Cancer 113, 2883–2891 (2008).
Pickering, L. M. et al. VinCaP: a phase II trial of vinflunine chemotherapy in locally-advanced and metastatic carcinoma of the penis (CRUK/12/021). J. Clin. Oncol. 36, 4514–4514 (2018).
Necchi, A. et al. First-line therapy with dacomitinib, an orally available pan-HER tyrosine kinase inhibitor, for locally advanced or metastatic penile squamous cell carcinoma: results of an open-label, single-arm, single-centre, phase 2 study. BJU Int. 121, 348–356 (2018).
Clark, P. E. et al. Penile cancer: clinical practice guidelines in oncology. J. Natl Compr. Cancer Netw. 11, 594–615 (2013).
Horton, R. H. & Lucassen, A. M. Recent developments in genetic/genomic medicine. Clin. Sci. 133, 697–708 (2019).
Subramaniam, D. S., Liu, S. V. & Giaccone, G. Novel approaches in cancer immunotherapy. Discov. Med. 21, 267–274 (2016).
Hsu, F. S., Su, C. H. & Huang, K. H. A comprehensive review of US FDA-approved immune checkpoint inhibitors in urothelial carcinoma. J. Immunol. Res. 2017, 6940546 (2017).
Helmink, B. A., Gaudreau, P. O. & Wargo, J. A. Immune checkpoint blockade across the cancer care continuum. Immunity 48, 1077–1080 (2018).
Motzer, R. J. et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N. Engl. J. Med. 378, 1277–1290 (2018).
Helmink, B. A., Khan, M. A. W., Hermann, A., Gopalakrishnan, V. & Wargo, J. A. The microbiome, cancer, and cancer therapy. Nat. Med. 25, 377–388 (2019).
Sivan, A. et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti-PD-L1 efficacy. Science 350, 1084–1089 (2015).
Viaud, S. et al. The intestinal microbiota modulates the anticancer immune effects of cyclophosphamide. Science 342, 971–976 (2013).
Backes, D. M., Kurman, R. J., Pimenta, J. M. & Smith, J. S. Systematic review of human papillomavirus prevalence in invasive penile cancer. Cancer Causes Control 20, 449–457 (2009).
Douglawi, A. & Masterson, T. A. Updates on the epidemiology and risk factors for penile cancer. Transl. Androl. Urol. 6, 785–790 (2017).
Stratton, M. R., Campbell, P. J. & Futreal, P. A. The cancer genome. Nature 458, 719–724 (2009).
Alves, G. et al. Genetic imbalances in 26 cases of penile squamous cell carcinoma. Genes Chromosomes Cancer 31, 48–53 (2001).
Poetsch, M., Schuart, B. J., Schwesinger, G., Kleist, B. & Protzel, C. Screening of microsatellite markers in penile cancer reveals differences between metastatic and nonmetastatic carcinomas. Mod. Pathol. 20, 1069–1077 (2007).
Busso-Lopes, A. F. et al. Genomic profiling of human penile carcinoma predicts worse prognosis and survival. Cancer Prev. Res. 8, 149–156 (2015).
Feber, A. et al. CSN1 somatic mutations in penile squamous cell carcinoma. Cancer Res. 76, 4720–4727 (2016).
Ceulemans, S., van der Ven, K. & Del-Favero, J. Targeted screening and validation of copy number variations. Methods Mol. Biol. 838, 311–328 (2012).
Li, W. & Olivier, M. Current analysis platforms and methods for detecting copy number variation. Physiol. Genomics 45, 1–16 (2013).
McDaniel, A. S. et al. Genomic profiling of penile squamous cell carcinoma reveals new opportunities for targeted therapy. Cancer Res. 75, 5219–5227 (2015).
Seed, G. et al. Gene copy number estimation from targeted next-generation sequencing of prostate cancer biopsies: analytic validation and clinical qualification. Clin. Cancer Res. 23, 6070–6077 (2017).
Hieronymus, H. et al. Tumor copy number alteration burden is a pan-cancer prognostic factor associated with recurrence and death. eLife 7, e37294 (2018).
Jacob, J. M. et al. Comparative genomic profiling of refractory and metastatic penile and nonpenile cutaneous squamous cell carcinoma: implications for selection of systemic therapy. J. Urol. 201, 541–548 (2019).
Tang, L. & Wang, K. Chronic inflammation in skin malignancies. J. Mol. Signal. 11, 2 (2016).
Halonen, P. et al. Lichen sclerosus and risk of cancer. Int. J. Cancer 140, 1998–2002 (2017).
Tezal, M. Interaction between chronic inflammation and oral HPV infection in the etiology of head and neck cancers. Int. J. Otolaryngol. 2012, 575242 (2012).
Powell, J. J. & Wojnarowska, F. Lichen sclerosus. Lancet 353, 1777–1783 (1999).
Philippou, P. et al. Genital lichen sclerosus/balanitis xerotica obliterans in men with penile carcinoma: a critical analysis. BJU Int. 111, 970–976 (2013).
Bazalinski, D., Przybek-Mita, J., Baranska, B. & Wiech, P. Marjolin’s ulcer in chronic wounds — review of available literature. Contemp. Oncol. 21, 197–202 (2017).
Green, A. C. & Olsen, C. M. Cutaneous squamous cell carcinoma: an epidemiological review. Br. J. Dermatol. 177, 373–381 (2017).
Eitsuka, T., Tatewaki, N., Nishida, H., Nakagawa, K. & Miyazawa, T. Synergistic anticancer effect of tocotrienol combined with chemotherapeutic agents or dietary components: a review. Int. J. Mol. Sci. 17, 1605 (2016).
Wieduwilt, M. J. & Moasser, M. M. The epidermal growth factor receptor family: biology driving targeted therapeutics. Cell Mol. Life Sci. 65, 1566–1584 (2008).
Scaltriti, M. & Baselga, J. The epidermal growth factor receptor pathway: a model for targeted therapy. Clin. Cancer Res. 12, 5268–5272 (2006).
Wang, S. & Li, J. Second-generation EGFR and ErbB tyrosine kinase inhibitors as first-line treatments for non-small cell lung cancer. Onco Targets Ther. 12, 6535–6548 (2019).
Sorich, M. J. et al. Extended RAS mutations and anti-EGFR monoclonal antibody survival benefit in metastatic colorectal cancer: a meta-analysis of randomized, controlled trials. Ann. Oncol. 26, 13–21 (2015).
Ali, S. M. et al. Comprehensive genomic profiling of advanced penile carcinoma suggests a high frequency of clinically relevant genomic alterations. Oncologist 21, 33–39 (2016).
Helsten, T. et al. The FGFR landscape in cancer: analysis of 4,853 tumors by next-generation sequencing. Clin. Cancer Res. 22, 259–267 (2016).
Fumarola, C. et al. Expanding the arsenal of FGFR inhibitors: a novel chloroacetamide derivative as a new irreversible agent with anti-proliferative activity against FGFR1-amplified lung cancer cell lines. Front. Oncol. 9, 179 (2019).
Konecny, G. E. & Kristeleit, R. S. PARP inhibitors for BRCA1/2-mutated and sporadic ovarian cancer: current practice and future directions. Br. J. Cancer 115, 1157–1173 (2016).
Yi, M. et al. Advances and perspectives of PARP inhibitors. Exp. Hematol. Oncol. 8, 29 (2019).
Jin, M. H. & Oh, D. Y. ATM in DNA repair in cancer. Pharmacol. Ther. 203, 107391 (2019).
Chen, C. C. et al. ATM loss leads to synthetic lethality in BRCA1 BRCT mutant mice associated with exacerbated defects in homology-directed repair. Proc. Natl Acad. Sci. USA 114, 7665–7670 (2017).
Cichowski, K. & Jacks, T. NF1 tumor suppressor gene function: narrowing the GAP. Cell 104, 593–604 (2001).
Zhu, Y. et al. Ablation of NF1 function in neurons induces abnormal development of cerebral cortex and reactive gliosis in the brain. Genes Dev. 15, 859–876 (2001).
Castellano, E. & Downward, J. RAS interaction with PI3K: more than just another effector pathway. Genes. Cancer 2, 261–274 (2011).
Yap, Y. S. et al. The NF1 gene revisited — from bench to bedside. Oncotarget 5, 5873–5892 (2014).
Gross, A. M. et al. Selumetinib in children with inoperable plexiform neurofibromas. N. Engl. J. Med. 382, 1430–1442 (2020).
Grimaldi, A. M. et al. MEK inhibitors in the treatment of metastatic melanoma and solid tumors. Am. J. Clin. Dermatol. 18, 745–754 (2017).
Hamada, K. et al. The PTEN/PI3K pathway governs normal vascular development and tumor angiogenesis. Genes Dev. 19, 2054–2065 (2005).
Tian, T., Li, X. & Zhang, J. mTOR signaling in cancer and mTOR inhibitors in solid tumor targeting therapy. Int. J. Mol. Sci. 20, 755 (2019).
Matsumoto, C. S. et al. PI3K-PTEN dysregulation leads to mTOR-driven upregulation of the core clock gene BMAL1 in normal and malignant epithelial cells. Oncotarget 7, 42393–42407 (2016).
Chavez-MacGregor, M. & Gonzalez-Angulo, A. M. Everolimus in the treatment of hormone receptor-positive breast cancer. Expert Opin. Investig. Drugs 21, 1835–1843 (2012).
Zhou, H., Luo, Y. & Huang, S. Updates of mTOR inhibitors. Anticancer Agents Med. Chem. 10, 571–581 (2010).
Andre, F. et al. Alpelisib for PIK3CA-mutated, hormone receptor-positive advanced breast cancer. N. Engl. J. Med. 380, 1929–1940 (2019).
Bader, A. G., Kang, S. & Vogt, P. K. Cancer-specific mutations in PIK3CA are oncogenic in vivo. Proc. Natl Acad. Sci. USA 103, 1475–1479 (2006).
Budzinska, M. A. et al. Accumulation of deleterious passenger mutations is associated with the progression of hepatocellular carcinoma. PLoS ONE 11, e0162586 (2016).
Kryukov, G. V., Pennacchio, L. A. & Sunyaev, S. R. Most rare missense alleles are deleterious in humans: implications for complex disease and association studies. Am. J. Hum. Genet. 80, 727–739 (2007).
Marchi, F. A. et al. Multidimensional integrative analysis uncovers driver candidates and biomarkers in penile carcinoma. Sci. Rep. 7, 6707 (2017).
Voges, Y. et al. Effects of YM155 on survivin levels and viability in neuroblastoma cells with acquired drug resistance. Cell Death Dis. 7, e2410 (2016).
Li, F., Aljahdali, I. & Ling, X. Cancer therapeutics using survivin BIRC5 as a target: what can we do after over two decades of study? J. Exp. Clin. Cancer Res. 38, 368 (2019).
Natale, R. et al. Evaluation of antitumor activity using change in tumor size of the survivin antisense oligonucleotide LY2181308 in combination with docetaxel for second-line treatment of patients with non-small-cell lung cancer: a randomized open-label phase II study. J. Thorac. Oncol. 9, 1704–1708 (2014).
Clemens, M. R. et al. Phase II, multicenter, open-label, randomized study of YM155 plus docetaxel as first-line treatment in patients with HER2-negative metastatic breast cancer. Breast Cancer Res. Treat. 149, 171–179 (2015).
Li, D., Hu, C. & Li, H. Survivin as a novel target protein for reducing the proliferation of cancer cells. Biomed. Rep. 8, 399–406 (2018).
Yamanaka, K. et al. Antitumor activity of YM155, a selective small-molecule survivin suppressant, alone and in combination with docetaxel in human malignant melanoma models. Clin. Cancer Res. 17, 5423–5431 (2011).
Decaudin, D. & Le Tourneau, C. Combinations of targeted therapies in human cancers. Aging 8, 2258–2259 (2016).
Johnson, D. B. et al. Combined BRAF (dabrafenib) and MEK inhibition (trametinib) in patients with BRAFV600-mutant melanoma experiencing progression with single-agent BRAF inhibitor. J. Clin. Oncol. 32, 3697–3704 (2014).
Blackwell, K. L. et al. Overall survival benefit with lapatinib in combination with trastuzumab for patients with human epidermal growth factor receptor 2-positive metastatic breast cancer: final results from the EGF104900 Study. J. Clin. Oncol. 30, 2585–2592 (2012).
Lim, S. Y., Menzies, A. M. & Rizos, H. Mechanisms and strategies to overcome resistance to molecularly targeted therapy for melanoma. Cancer 123, 2118–2129 (2017).
Olesen, T. B. et al. Prevalence of human papillomavirus DNA and p16INK4a in penile cancer and penile intraepithelial neoplasia: a systematic review and meta-analysis. Lancet Oncol. 20, 145–158 (2019).
Mannweiler, S., Sygulla, S., Winter, E. & Regauer, S. Two major pathways of penile carcinogenesis: HPV-induced penile cancers overexpress p16ink4a, HPV-negative cancers associated with dermatoses express p53, but lack p16ink4a overexpression. J. Am. Acad. Dermatol. 69, 73–81 (2013).
Sharpless, N. E. & DePinho, R. A. The INK4A/ARF locus and its two gene products. Curr. Opin. Genet. Dev. 9, 22–30 (1999).
Rivlin, N., Brosh, R., Oren, M. & Rotter, V. Mutations in the p53 tumor suppressor gene: important milestones at the various steps of tumorigenesis. Genes Cancer 2, 466–474 (2011).
Hall, P. A. & Lane, D. P. p53 in tumour pathology: can we trust immunohistochemistry? Revisited! J. Pathol. 172, 1–4 (1994).
Rocha, R. M. et al. A clinical, pathologic, and molecular study of p53 and murine double minute 2 in penile carcinogenesis and its relation to prognosis. Hum. Pathol. 43, 481–488 (2012).
Zhang, J. et al. Prognostic significance of p16INK4a expression in penile squamous cell carcinoma: a meta-analysis with trial sequential analysis. Biomed. Res. Int. 2018, 8345893 (2018).
Albers, A. E., Qian, X., Kaufmann, A. M. & Coordes, A. Meta analysis: HPV and p16 pattern determines survival in patients with HNSCC and identifies potential new biologic subtype. Sci. Rep. 7, 16715 (2017).
Lin, J., Albers, A. E., Qin, J. & Kaufmann, A. M. Prognostic significance of overexpressed p16INK4a in patients with cervical cancer: a meta-analysis. PLoS ONE 9, e106384 (2014).
Sun, G. et al. The prognostic value of HPV combined p16 status in patients with anal squamous cell carcinoma: a meta-analysis. Oncotarget 9, 8081–8088 (2018).
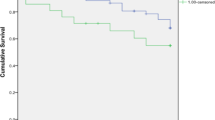
Sand, F. L., Rasmussen, C. L., Frederiksen, M. H., Andersen, K. K. & Kjaer, S. K. Prognostic significance of HPV and p16 status in men diagnosed with penile cancer: a systematic review and meta-analysis. Cancer Epidemiol. Biomarkers Prev. 27, 1123–1132 (2018).
Davis, A., Gao, R. & Navin, N. Tumor evolution: linear, branching, neutral or punctuated? Biochim. Biophys. Acta Rev. Cancer 1867, 151–161 (2017).
Chahoud, J. et al. Penile squamous cell carcinoma is genomically similar to other HPV-driven tumors. J. Clin. Oncol. 37, 505–505 (2019).
Jacob, J. et al. Penile and uterine cervical squamous cell carcinomas: a comparative genomic profiling study. J. Clin. Oncol. 37, 514–514 (2019).
Tward, J. The case for nonsurgical therapy of nonmetastatic penile cancer. Nat. Rev. Urol. 15, 574–584 (2018).
Stankiewicz, E. et al. Alternative HER/PTEN/Akt pathway activation in HPV positive and negative penile carcinomas. PLoS ONE 6, e17517 (2011).
Hafner, N. et al. Integration of the HPV16 genome does not invariably result in high levels of viral oncogene transcripts. Oncogene 27, 1610–1617 (2008).
Ghittoni, R. et al. The biological properties of E6 and E7 oncoproteins from human papillomaviruses. Virus Genes 40, 1–13 (2010).
Hoppe-Seyler, K., Bossler, F., Braun, J. A., Herrmann, A. L. & Hoppe-Seyler, F. The HPV E6/E7 oncogenes: key factors for viral carcinogenesis and therapeutic targets. Trends Microbiol. 26, 158–168 (2018).
Martinez-Zapien, D. et al. Structure of the E6/E6AP/p53 complex required for HPV-mediated degradation of p53. Nature 529, 541–545 (2016).
Chabeda, A. et al. Therapeutic vaccines for high-risk HPV-associated diseases. Papillomavirus Res. 5, 46–58 (2018).
Hung, C. F., Ma, B., Monie, A., Tsen, S. W. & Wu, T. C. Therapeutic human papillomavirus vaccines: current clinical trials and future directions. Expert Opin. Biol. Ther. 8, 421–439 (2008).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02426892 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02858310 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03418480 (2020).
Qin, Y. et al. Cervical cancer neoantigen landscape and immune activity is associated with human papillomavirus master regulators. Front. Immunol. 8, 689 (2017).
Kumar, D. et al. Integrating transcriptome and proteome profiling: strategies and applications. Proteomics 16, 2533–2544 (2016).
Manzoni, C. et al. Genome, transcriptome and proteome: the rise of omics data and their integration in biomedical sciences. Brief. Bioinform. 19, 286–302 (2018).
Kuasne, H. et al. Genome-wide methylation and transcriptome analysis in penile carcinoma: uncovering new molecular markers. Clin. Epigenetics 7, 46 (2015).
Frohlich, E. & Wahl, R. Chemotherapy and chemoprevention by thiazolidinediones. Biomed. Res. Int. 2015, 845340 (2015).
Kuasne, H. et al. Integrative miRNA and mRNA analysis in penile carcinomas reveals markers and pathways with potential clinical impact. Oncotarget 8, 15294–15306 (2017).
Mueller, E. et al. Effects of ligand activation of peroxisome proliferator-activated receptor gamma in human prostate cancer. Proc. Natl Acad. Sci. USA 97, 10990–10995 (2000).
Khodarev, N. N., Roizman, B. & Weichselbaum, R. R. Molecular pathways: interferon/STAT1 pathway: role in the tumor resistance to genotoxic stress and aggressive growth. Clin. Cancer Res. 18, 3015–3021 (2012).
Schwartz, D. M. et al. JAK inhibition as a therapeutic strategy for immune and inflammatory diseases. Nat. Rev. Drug Discov. 17, 78 (2017).
Fetter, T. et al. Selective Janus kinase 1 inhibition is a promising therapeutic approach for lupus erythematosus skin lesions. Front. Immunol. 11, 344 (2020).
Saeed, S., Keehn, C. A., Khalil, F. K. & Morgan, M. B. Immunohistochemical expression of Bax and Bcl-2 in penile carcinoma. Ann. Clin. Lab. Sci. 35, 91–96 (2005).
Brown, V. L. et al. p16INK4a and p14ARF tumor suppressor genes are commonly inactivated in cutaneous squamous cell carcinoma. J. Invest. Dermatol. 122, 1284–1292 (2004).
Kuasne, H., Marchi, F. A., Rogatto, S. R. & de Syllos Colus, I. M. Epigenetic mechanisms in penile carcinoma. Int. J. Mol. Sci. 14, 10791–10808 (2013).
Ferreux, E. et al. Evidence for at least three alternative mechanisms targeting the p16INK4A/cyclin D/Rb pathway in penile carcinoma, one of which is mediated by high-risk human papillomavirus. J. Pathol. 201, 109–118 (2003).
Yanagawa, N., Osakabe, M., Hayashi, M., Tamura, G. & Motoyama, T. Detection of HPV-DNA, p53 alterations, and methylation in penile squamous cell carcinoma in Japanese men. Pathol. Int. 58, 477–482 (2008).
Poetsch, M. et al. Alterations in the tumor suppressor gene p16INK4A are associated with aggressive behavior of penile carcinomas. Virchows Arch. 458, 221–229 (2011).
Lu, J. et al. MicroRNA expression profiles classify human cancers. Nature 435, 834–838 (2005).
Nelson, P. T. et al. Microarray-based, high-throughput gene expression profiling of microRNAs. Nat. Methods 1, 155–161 (2004).
Zhang, L. et al. MicroRNA expression profile in penile cancer revealed by next-generation small RNA sequencing. PLoS ONE 10, e0131336 (2015).
Barzon, L. et al. Profiling of expression of human papillomavirus-related cancer miRNAs in penile squamous cell carcinomas. Am. J. Pathol. 184, 3376–3383 (2014).
Kuasne, H. et al. Nuclear loss and cytoplasmic expression of androgen receptor in penile carcinomas: role as a driver event and as a prognosis factor. Virchows Arch. 473, 607–614 (2018).
Li, X. J., Ren, Z. J. & Tang, J. H. MicroRNA-34a: a potential therapeutic target in human cancer. Cell Death Dis. 5, e1327 (2014).
Chaux, A. et al. Comparison of morphologic features and outcome of resected recurrent and nonrecurrent squamous cell carcinoma of the penis: a study of 81 cases. Am. J. Surg. Pathol. 33, 1299–1306 (2009).
Kattan, M. W. et al. Nomogram predictive of cancer specific survival in patients undergoing partial or total amputation for squamous cell carcinoma of the penis. J. Urol. 175, 2103–2108 (2006).
Grabowski, P., Kustatscher, G. & Rappsilber, J. Epigenetic variability confounds transcriptome but not proteome profiling for coexpression-based gene function prediction. Mol. Cell Proteom. 17, 2082–2090 (2018).
Dix, B., Robbins, P., Carrello, S., House, A. & Iacopetta, B. Comparison of p53 gene mutation and protein overexpression in colorectal carcinomas. Br. J. Cancer 70, 585–590 (1994).
Li, A. R. et al. EGFR mutations in lung adenocarcinomas: clinical testing experience and relationship to EGFR gene copy number and immunohistochemical expression. J. Mol. Diagn. 10, 242–248 (2008).
Kitamura, A., Hosoda, W., Sasaki, E., Mitsudomi, T. & Yatabe, Y. Immunohistochemical detection of EGFR mutation using mutation-specific antibodies in lung cancer. Clin. Cancer Res. 16, 3349–3355 (2010).
Sholl, L. M. et al. EGFR mutation is a better predictor of response to tyrosine kinase inhibitors in non-small cell lung carcinoma than FISH, CISH, and immunohistochemistry. Am. J. Clin. Pathol. 133, 922–934 (2010).
Lehmann-Che, J. et al. Immunohistochemical and molecular analyses of HER2 status in breast cancers are highly concordant and complementary approaches. Br. J. Cancer 104, 1739–1746 (2011).
Kuboki, Y. et al. Comprehensive analyses using next-generation sequencing and immunohistochemistry enable precise treatment in advanced gastric cancer. Ann. Oncol. 27, 127–133 (2016).
Lopes, A. et al. p53 as a new prognostic factor for lymph node metastasis in penile carcinoma: analysis of 82 patients treated with amputation and bilateral lymphadenectomy. J. Urol. 168, 81–86 (2002).
Martins, A. C., Faria, S. M., Cologna, A. J., Suaid, H. J. & Tucci, S. Jr. Immunoexpression of p53 protein and proliferating cell nuclear antigen in penile carcinoma. J. Urol. 167, 89–92 (2002).
Zargar-Shoshtari, K. et al. Clinical significance of p53 and p16INK4A status in a contemporary North American penile carcinoma cohort. Clin. Genitourin. Cancer 14, 346–351 (2016).
Liu, J. Y. et al. The risk factors for the presence of pelvic lymph node metastasis in penile squamous cell carcinoma patients with inguinal lymph node dissection. World J. Urol. 31, 1519–1524 (2013).
Zargar-Shoshtari, K., Sharma, P. & Spiess, P. E. Insight into novel biomarkers in penile cancer: redefining the present and future treatment paradigm? Urol. Oncol. 36, 433–439 (2018).
Laniado, M. E., Lowdell, C., Mitchell, H. & Christmas, T. J. Squamous cell carcinoma antigen: a role in the early identification of nodal metastases in men with squamous cell carcinoma of the penis. BJU Int. 92, 248–250 (2003).
Zhu, Y., Zhou, X. Y., Yao, X. D., Dai, B. & Ye, D. W. The prognostic significance of p53, Ki-67, epithelial cadherin and matrix metalloproteinase-9 in penile squamous cell carcinoma treated with surgery. BJU Int. 100, 204–208 (2007).
Steffens, S. et al. High CRP values predict poor survival in patients with penile cancer. BMC Cancer 13, 223 (2013).
Rosenberg, J. E. et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet 387, 1909–1920 (2016).
Attalla, K., Sfakianos, J. P. & Galsky, M. D. Current role of checkpoint inhibitors in urologic cancers. Cancer Treat. Res. 175, 241–258 (2018).
Ottenhof, S. R. et al. Expression of programmed death ligand 1 in penile cancer is of prognostic value and associated with HPV status. J. Urol. 197, 690–697 (2017).
Udager, A. M. et al. Frequent PD-L1 expression in primary and metastatic penile squamous cell carcinoma: potential opportunities for immunotherapeutic approaches. Ann. Oncol. 27, 1706–1712 (2016).
Cocks, M. et al. Immune-checkpoint status in penile squamous cell carcinoma: a North American cohort. Hum. Pathol. 59, 55–61 (2017).
Udall, M. et al. PD-L1 diagnostic tests: a systematic literature review of scoring algorithms and test-validation metrics. Diagn. Pathol. 13, 12 (2018).
Ottenhof, S. R. et al. The prognostic value of immune factors in the tumor microenvironment of penile squamous cell carcinoma. Front. Immunol. 9, 1253 (2018).
Cheng, Z., Zhang, D., Gong, B., Wang, P. & Liu, F. CD163 as a novel target gene of STAT3 is a potential therapeutic target for gastric cancer. Oncotarget 8, 87244–87262 (2017).
Garvin, S., Oda, H., Arnesson, L. G., Lindstrom, A. & Shabo, I. Tumor cell expression of CD163 is associated to postoperative radiotherapy and poor prognosis in patients with breast cancer treated with breast-conserving surgery. J. Cancer Res. Clin. Oncol. 144, 1253–1263 (2018).
Buechler, C. et al. Regulation of scavenger receptor CD163 expression in human monocytes and macrophages by pro- and antiinflammatory stimuli. J. Leukoc. Biol. 67, 97–103 (2000).
Maniecki, M. B. et al. Tumor-promoting macrophages induce the expression of the macrophage-specific receptor CD163 in malignant cells. Int. J. Cancer 131, 2320–2331 (2012).
Qian, B. Z. & Pollard, J. W. Macrophage diversity enhances tumor progression and metastasis. Cell 141, 39–51 (2010).
Gooden, M. J., de Bock, G. H., Leffers, N., Daemen, T. & Nijman, H. W. The prognostic influence of tumour-infiltrating lymphocytes in cancer: a systematic review with meta-analysis. Br. J. Cancer 105, 93–103 (2011).
Peranzoni, E. et al. Macrophages impede CD8 T cells from reaching tumor cells and limit the efficacy of anti-PD-1 treatment. Proc. Natl Acad. Sci. USA 115, E4041–E4050 (2018).
Hennequart, M. et al. Constitutive IDO1 expression in human tumors is driven by cyclooxygenase-2 and mediates intrinsic immune resistance. Cancer Immunol. Res. 5, 695–709 (2017).
Golijanin, D. et al. Cyclooxygenase-2 and microsomal prostaglandin E synthase-1 are overexpressed in squamous cell carcinoma of the penis. Clin. Cancer Res. 10, 1024–1031 (2004).
Surace, M. et al. Automated multiplex immunofluorescence panel for immuno-oncology studies on formalin-fixed carcinoma tissue specimens. J. Vis. Exp. 143, e58390 (2019).
Feng, Z. et al. Multiparametric immune profiling in HPV-oral squamous cell cancer. JCI Insight 2, e93652 (2017).
Galon, J. et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 313, 1960–1964 (2006).
Bethmann, D., Feng, Z. & Fox, B. A. Immunoprofiling as a predictor of patient’s response to cancer therapy — promises and challenges. Curr. Opin. Immunol. 45, 60–72 (2017).
Gibney, G. T., Weiner, L. M. & Atkins, M. B. Predictive biomarkers for checkpoint inhibitor-based immunotherapy. Lancet Oncol. 17, e542–e551 (2016).
Chalmers, Z. R. et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 9, 34 (2017).
Chang, L., Chang, M., Chang, H. M. & Chang, F. Microsatellite instability: a predictive biomarker for cancer immunotherapy. Appl. Immunohistochem. Mol. Morphol. 26, e15–e21 (2018).
Ratti, M., Lampis, A., Hahne, J. C., Passalacqua, R. & Valeri, N. Microsatellite instability in gastric cancer: molecular bases, clinical perspectives, and new treatment approaches. Cell Mol. Life Sci. 75, 4151–4162 (2018).
Le, D. T. et al. Phase II open-label study of pembrolizumab in treatment-refractory, microsatellite instability-high/mismatch repair-deficient metastatic colorectal cancer: KEYNOTE-164. J. Clin. Oncol. 38, 11–19 (2020).
Llosa, N. J. et al. The vigorous immune microenvironment of microsatellite instable colon cancer is balanced by multiple counter-inhibitory checkpoints. Cancer Discov. 5, 43–51 (2015).
Champiat, S. et al. Hyperprogressive disease is a new pattern of progression in cancer patients treated by anti-PD-1/PD-L1. Clin. Cancer Res. 23, 1920–1928 (2017).
Singavi, A. K. et al. Predictive biomarkers for hyper-progression (HP) in response to immune checkpoint inhibitors (ICI): analysis of somatic alterations (SAs). Ann. Oncol. 28(Suppl.5), v403–v427 (2017).
Kato, S. et al. Hyperprogressors after immunotherapy: analysis of genomic alterations associated with accelerated growth rate. Clin. Cancer Res. 23, 4242–4250 (2017).
Wade, M., Li, Y. C. & Wahl, G. M. MDM2, MDMX and p53 in oncogenesis and cancer therapy. Nat. Rev. Cancer 13, 83–96 (2013).
Koyama, S. et al. STK11/LKB1 deficiency promotes neutrophil recruitment and proinflammatory cytokine production to suppress T-cell activity in the lung tumor microenvironment. Cancer Res. 76, 999–1008 (2016).
Skoulidis, F. et al. STK11/LKB1 mutations and PD-1 inhibitor resistance in KRAS-mutant lung adenocarcinoma. Cancer Discov. 8, 822–835 (2018).
Migden, M. R. et al. PD-1 blockade with cemiplimab in advanced cutaneous squamous-cell carcinoma. N. Engl. J. Med. 379, 341–351 (2018).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03391479 (2019).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT03686332 (2019).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02834013 (2020).
US National Library of Medicine. ClinicalTrials.gov https://clinicaltrials.gov/ct2/show/NCT02496208 (2020).
Lu, X. et al. Effective combinatorial immunotherapy for castration-resistant prostate cancer. Nature 543, 728–732 (2017).
Bhatt, A. P., Redinbo, M. R. & Bultman, S. J. The role of the microbiome in cancer development and therapy. CA Cancer J. Clin. 67, 326–344 (2017).
Goedert, J. J. et al. Fecal microbiota characteristics of patients with colorectal adenoma detected by screening: a population-based study. EBioMedicine 2, 597–603 (2015).
Urbaniak, C. et al. The microbiota of breast tissue and its association with breast cancer. Appl. Env. Microbiol. 82, 5039–5048 (2016).
Heshiki, Y. et al. Predictable modulation of cancer treatment outcomes by the gut microbiota. Microbiome 8, 28 (2020).
Matson, V. et al. The commensal microbiome is associated with anti-PD-1 efficacy in metastatic melanoma patients. Science 359, 104–108 (2018).
Consoli, M. L. et al. Randomized clinical trial: impact of oral administration of Saccharomyces boulardii on gene expression of intestinal cytokines in patients undergoing colon resection. J. Parenter. Enter. Nutr. 40, 1114–1121 (2016).
Laniewski, P., Ilhan, Z. E. & Herbst-Kralovetz, M. M. The microbiome and gynaecological cancer development, prevention and therapy. Nat. Rev. Urol. 17, 232–250 (2020).
Norenhag, J. et al. The vaginal microbiota, human papillomavirus and cervical dysplasia: a systematic review and network meta-analysis. BJOG 127, 171–180 (2020).
Chao, X. P. et al. Correlation between the diversity of vaginal microbiota and the risk of high-risk human papillomavirus infection. Int. J. Gynecol. Cancer 29, 28–34 (2019).
Liu, C. M. et al. Penile anaerobic dysbiosis as a risk factor for HIV infection. MBio 8, e00996-17 (2017).
Price, L. B. et al. The effects of circumcision on the penis microbiome. PLoS ONE 5, e8422 (2010).
Gopalakrishnan, V., Helmink, B. A., Spencer, C. N., Reuben, A. & Wargo, J. A. The influence of the gut microbiome on cancer, immunity, and cancer immunotherapy. Cancer Cell 33, 570–580 (2018).
Onywera, H. et al. The penile microbiota of black South African men: relationship with human papillomavirus and HIV infection. BMC Microbiol. 20, 78 (2020).
Weinstock, G. M. Genomic approaches to studying the human microbiota. Nature 489, 250–256 (2012).
Group, N. H. W. et al. The NIH human microbiome project. Genome Res. 19, 2317–2323 (2009).
Author information
Authors and Affiliations
Contributions
A.M.A. and P.E.S. researched data for the article. A.M.A. and J.C. made substantial contributions to discussion of the article content. A.M.A. and J.J.A. wrote the manuscript. All authors reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
J.S.R.: employment: Foundation Medicine; leadership: Foundation Medicine; stock and other ownership interests: Foundation Medicine; research funding: Foundation Medicine. A.N.: employment: Bayer A.G.; stock and other ownership interests: Bayer A.G.; honoraria: Roche Merck, AstraZeneca, Janssen Pharmaceuticals, and Foundation Medicine; consulting or advisory role: Merck Sharp & Dohme, Roche, Bayer A.G., AstraZeneca, Clovis Oncology, Janssen Pharmaceuticals, Incyte, Seattle Genetics, Astellas Pharma, Bristol-Myers Squibb and Rainier Therapeutics; research funding: Merck Sharp & Dohme (to the institute) and AstraZeneca (to the institute); travel, accommodations, expenses: Roche, Merck Sharp & Dohme, AstraZeneca and Janssen Pharmaceuticals. P.E.S.: consulting or advisory role: Genentech and Pfizer. A.M.A., J.C., J.J.A., M.A. and A.M. declare no competing interests.
Additional information
Peer review information
Nature Reviews Urology thanks M. Albersen, M. Burger and J. Tward for their contribution to the peer review of this work.
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Aydin, A.M., Chahoud, J., Adashek, J.J. et al. Understanding genomics and the immune environment of penile cancer to improve therapy. Nat Rev Urol 17, 555–570 (2020). https://doi.org/10.1038/s41585-020-0359-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41585-020-0359-z
This article is cited by
-
SPP1 is associated with adverse prognosis and predicts immunotherapy efficacy in penile cancer
Human Genomics (2023)
-
Immune-based therapies in penile cancer
Nature Reviews Urology (2022)
-
A comprehensive analysis of penile cancer in the region with the highest worldwide incidence reveals new insights into the disease
BMC Cancer (2022)
-
Penile cancer
Nature Reviews Disease Primers (2021)