Abstract
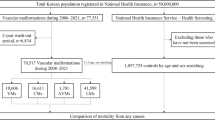
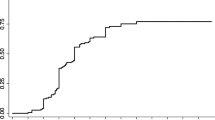
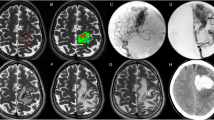
An arteriovenous malformation is a tangle of dysplastic vessels (nidus) fed by arteries and drained by veins without intervening capillaries, forming a high-flow, low-resistance shunt between the arterial and venous systems. Arteriovenous malformations in the brain have a low estimated prevalence but are an important cause of intracerebral haemorrhage in young adults. For previously unruptured malformations, bleeding rates are approximately 1% per year. Once ruptured, the subsequent risk increases fivefold, depending on associated aneurysms, deep locations, deep drainage and increasing age. Recent findings from novel animal models and genetic studies suggest that arteriovenous malformations, which were long considered congenital, arise from aberrant vasculogenesis, genetic mutations and/or angiogenesis after injury. The phenotypical characteristics of arteriovenous malformations differ among age groups, with fistulous lesions in children and nidal lesions in adults. Diagnosis mainly involves imaging techniques, including CT, MRI and angiography. Management includes observation, microsurgical resection, endovascular embolization and stereotactic radiosurgery, alone or in any combination. There is little consensus on how to manage patients with unruptured malformations; recent studies have shown that patients managed medically fared better than those with intervention at short-term follow-up. By contrast, interventional treatment is preferred following a ruptured malformation to prevent rehaemorrhage. Management continues to evolve as new mechanistic discoveries and reliable animal models raise the possibility of developing drugs that might prevent the formation of arteriovenous malformations, induce obliteration and/or stabilize vessels to reduce rupture risk. For an illustrated summary of this Primer, visit: http://go.nature.com/TMoAdn
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 1 digital issues and online access to articles
$99.00 per year
only $99.00 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout









Similar content being viewed by others
References
Morris, Z. et al. Incidental findings on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ 339, b3016 (2009).
Stapf, C. et al. The New York Islands AVM Study: design, study progress, and initial results. Stroke 34, e29–e33 (2003).
Stapf, C. et al. Incidence of adult brain arteriovenous malformation hemorrhage in a prospective population-based stroke survey. Cerebrovasc. Dis. 13, 43–46 (2002).
Al-Shahi, R. et al. Prospective, population-based detection of intracranial vascular malformations in adults: the Scottish Intracranial Vascular Malformation Study (SIVMS). Stroke 34, 1163–1169 (2003).
Gabriel, R. A. et al. Ten-year detection rate of brain arteriovenous malformations in a large, multiethnic, defined population. Stroke 41, 21–26 (2010).
Hofmeister, C. et al. Demographic, morphological, and clinical characteristics of 1289 patients with brain arteriovenous malformation. Stroke 31, 1307–1310 (2000).
ApSimon, H. T., Reef, H., Phadke, R. V. & Popovic, E. A. A population-based study of brain arteriovenous malformation: long-term treatment outcomes. Stroke 33, 2794–2800 (2002).
Crawford, P. M., West, C. R., Chadwick, D. W. & Shaw, M. D. Arteriovenous malformations of the brain: natural history in unoperated patients. J. Neurol. Neurosurg. Psychiatry 49, 1–10 (1986).
Ondra, S. L., Troupp, H., George, E. D. & Schwab, K. The natural history of symptomatic arteriovenous malformations of the brain: a 24-year follow-up assessment. J. Neurosurg. 73, 387–391 (1990). A study of haemorrhage rates associated with untreated arteriovenous malformations in a controlled population in Finland, establishing some of the best natural history data on this condition.
Englot, D. J. et al. Seizure predictors and control after microsurgical resection of supratentorial arteriovenous malformations in 440 patients. Neurosurgery 71, 572–580; discussion 580 (2012).
Fults, D. & Kelly, D. L. Jr. Natural history of arteriovenous malformations of the brain: a clinical study. Neurosurgery 15, 658–662 (1984).
Kim, H., Al- Shahi Salman, R., McCulloch, C. E., Stapf, C. & Young, W. L. Untreated brain arteriovenous malformation: patient-level meta-analysis of hemorrhage predictors. Neurology 83, 590–597 (2014). This paper combined four separate cohorts to show that increasing age and presentation with bleeding were predictors of arteriovenous malformation haemorrhage.
Mohr, J. P. et al. Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, non-blinded, randomised trial. Lancet 383, 614–621 (2014). This randomized clinical trial compared various therapeutic interventions to medical management and its results have stirred worldwide debate about arteriovenous malformation management.
Halim, A. X. et al. Longitudinal risk of intracranial hemorrhage in patients with arteriovenous malformation of the brain within a defined population. Stroke 35, 1697–1702 (2004).
Hernesniemi, J. A. et al. Natural history of brain arteriovenous malformations: a long-term follow-up study of risk of hemorrhage in 238 patients. Neurosurgery 63, 823–829; discussion 829–831 (2008).
Kim, H. et al. Racial/ethnic differences in longitudinal risk of intracranial hemorrhage in brain arteriovenous malformation patients. Stroke 38, 2430–2437 (2007).
Stapf, C. et al. Predictors of hemorrhage in patients with untreated brain arteriovenous malformation. Neurology 66, 1350–1355 (2006). This study showed that arteriovenous malformations in deep locations, with deep venous drainage and presenting with previous haemorrhage could have rupture rates as high as 35% per year.
Guo, Y. et al. Silent intralesional microhemorrhage as a risk factor for brain arteriovenous malformation rupture. Stroke 43, 1240–1246 (2012).
Liu, X. J. et al. Risk of cerebral arteriovenous malformation rupture during pregnancy and puerperium. Neurology 82, 1798–1803 (2014).
van Beijnum, J. et al. Prevalence of brain arteriovenous malformations in first-degree relatives of patients with a brain arteriovenous malformation. Stroke 45, 3231–3235 (2014).
van Beijnum, J. et al. Outcome after spontaneous and arteriovenous malformation-related intracerebral haemorrhage: population-based studies. Brain 132, 537–543 (2009).
Laakso, A. et al. Long-term excess mortality in 623 patients with brain arteriovenous malformations. Neurosurgery 63, 244–253; discussion 253–255 (2008).
Wedderburn, C. J. et al. Outcome after interventional or conservative management of unruptured brain arteriovenous malformations: a prospective, population-based cohort study. Lancet Neurol. 7, 223–230 (2008).
Al-Shahi Salman, R. et al. Outcome after conservative management or intervention for unruptured brain arteriovenous malformations. JAMA 311, 1661–1669 (2014). This study of a cohort in Scotland corroborated findings from the ARUBA trial, adding to the controversy relating to the management of arteriovenous malformation.
Josephson, C. B. et al. Seizure risk with AVM treatment or conservative management: prospective, population-based study. Neurology 79, 500–507 (2012).
Lawton, M. T., Jacobowitz, R. & Spetzler, R. F. Redefined role of angiogenesis in the pathogenesis of dural arteriovenous malformations. J. Neurosurg. 87, 267–274 (1997).
Risau, W. Mechanisms of angiogenesis. Nature 386, 671–674 (1997).
Kume, T. Specification of arterial, venous, and lymphatic endothelial cells during embryonic development. Histol. Histopathol. 25, 637–646 (2010).
Gerety, S. S. & Anderson, D. J. Cardiovascular ephrinB2 function is essential for embryonic angiogenesis. Development 129, 1397–1410 (2002).
Swift, M. R. & Weinstein, B. M. Arterial-venous specification during development. Circ. Res. 104, 576–588 (2009).
Mukouyama, Y. S., Shin, D., Britsch, S., Taniguchi, M. & Anderson, D. J. Sensory nerves determine the pattern of arterial differentiation and blood vessel branching in the skin. Cell 109, 693–705 (2002).
Moyon, D., Pardanaud, L., Yuan, L., Breant, C. & Eichmann, A. Plasticity of endothelial cells during arterial-venous differentiation in the avian embryo. Development 128, 3359–3370 (2001).
Sorensen, I., Adams, R. H. & Gossler, A. DLL1-mediated Notch activation regulates endothelial identity in mouse fetal arteries. Blood 113, 5680–5688 (2009).
Lawson, N. D., Vogel, A. M. & Weinstein, B. M. sonic hedgehog and vascular endothelial growth factor act upstream of the Notch pathway during arterial endothelial differentiation. Dev. Cell 3, 127–136 (2002).
Hayashi, H. & Kume, T. Foxc transcription factors directly regulate Dll4 and Hey2 expression by interacting with the VEGF–Notch signaling pathways in endothelial cells. PLoS ONE 3, e2401 (2008).
Shoemaker, L. D. et al. Human brain arteriovenous malformations express lymphatic-associated genes. Ann. Clin. Transl. Neurol. 1, 982–995 (2014).
You, L. R. et al. Suppression of Notch signalling by the COUP-TFII transcription factor regulates vein identity. Nature 435, 98–104 (2005).
Faughnan, M. E. et al. International guidelines for the diagnosis and management of hereditary haemorrhagic telangiectasia. J. Med. Genet. 48, 73–87 (2011).
McAllister, K. A. et al. Endoglin, a TGF-β bindinG protein of endothelial cells, is the gene for hereditary haemorrhagic telangiectasia type 1. Nat. Genet. 8, 345–351 (1994). This paper describes the genetic basis of arteriovenous malformations in hereditary haemorrhagic telangiectasia.
Johnson, D. W. et al. Mutations in the activin receptor-like kinase 1 gene in hereditary haemorrhagic telangiectasia type 2. Nat. Genet. 13, 189–195 (1996). This manuscript established the genetic basis for arteriovenous malformations in hereditary haemorrhagic telangiectasia and guided the development of animal models.
Govani, F. S. & Shovlin, C. L. Hereditary haemorrhagic telangiectasia: a clinical and scientific review. Eur. J. Hum. Genet. 17, 860–871 (2009).
Gallione, C. J. et al. A combined syndrome of juvenile polyposis and hereditary haemorrhagic telangiectasia associated with mutations in MADH4 (SMAD4). Lancet 363, 852–859 (2004).
David, L., Mallet, C., Mazerbourg, S., Feige, J. J. & Bailly, S. Identification of BMP9 and BMP10 as functional activators of the orphan activin receptor-like kinase 1 (ALK1) in endothelial cells. Blood 109, 1953–1961 (2007).
David, L. et al. Bone morphogenetic protein-9 is a circulating vascular quiescence factor. Circ. Res. 102, 914–922 (2008).
Wooderchak-Donahue, W. L. et al. BMP9 mutations cause a vascular-anomaly syndrome with phenotypic overlap with hereditary hemorrhagic telangiectasia. Am. J. Hum. Genet. 93, 530–537 (2013).
Dupuis-Girod, S. et al. Bevacizumab in patients with hereditary hemorrhagic telangiectasia and severe hepatic vascular malformations and high cardiac output. JAMA 307, 948–955 (2012).
Flieger, D., Hainke, S. & Fischbach, W. Dramatic improvement in hereditary hemorrhagic telangiectasia after treatment with the vascular endothelial growth factor (VEGF) antagonist bevacizumab. Ann. Hematol. 85, 631–632 (2006).
Sorensen, L. K., Brooke, B. S., Li, D. Y. & Urness, L. D. Loss of distinct arterial and venous boundaries in mice lacking endoglin, a vascular-specific TGFβ coreceptor. Dev. Biol. 261, 235–250 (2003).
Urness, L. D., Sorensen, L. K. & Li, D. Y. Arteriovenous malformations in mice lacking activin receptor-like kinase-1. Nat. Genet. 26, 328–331 (2000).
Park, S. O. et al. Real-time imaging of de novo arteriovenous malformation in a mouse model of hereditary hemorrhagic telangiectasia. J. Clin. Invest. 119, 3487–3496 (2009).
Garrido-Martin, E. M. et al. Common and distinctive pathogenetic features of arteriovenous malformations in hereditary hemorrhagic telangiectasia 1 and hereditary hemorrhagic telangiectasia 2 animal models — brief report. Arterioscler. Thromb. Vasc. Biol. 34, 2232–2236 (2014).
Boon, L. M., Mulliken, J. B. & Vikkula, M. RASA1: variable phenotype with capillary and arteriovenous malformations. Curr. Opin. Genet. Dev. 15, 265–269 (2005).
Kawasaki, J. et al. RASA1 functions in EPHB4 signaling pathway to suppress endothelial mTORC1 activity. J. Clin. Invest. 124, 2774–2784 (2014).
Shirley, M. D. et al. Sturge–Weber syndrome and port-wine stains caused by somatic mutation in GNAQ. N. Engl. J. Med. 368, 1971–1979 (2013).
Hong, C. C., Peterson, Q. P., Hong, J. Y. & Peterson, R. T. Artery/vein specification is governed by opposing phosphatidylinositol-3 kinase and MAP kinase/ERK signaling. Curr. Biol. 16, 1366–1372 (2006).
Pawlikowska, L. et al. Polymorphisms in transforming growth factor-B-related genes ALK1 and ENG are associated with sporadic brain arteriovenous malformations. Stroke 36, 2278–2280 (2005).
Young, W. L. et al. Arteriovenous malformation. J. Neurosurg. 106, 731–732 (2007).
Simon, M. et al. Association of a polymorphism of the ACVRL1 gene with sporadic arteriovenous malformations of the central nervous system. J. Neurosurg. 104, 945–949 (2006).
Su, H. et al. Reduced expression of integrin αvβ8 is associated with brain arteriovenous malformation pathogenesis. Am. J. Pathol. 176, 1018–1027 (2010).
Kim, H. et al. Common variants in interleukin-1-β gene are associated with intracranial hemorrhage and susceptibility to brain arteriovenous malformation. Cerebrovasc. Dis. 27, 176–182 (2009).
Mikhak, B. et al. Angiopoietin-like 4 (ANGPTL4) gene polymorphisms and risk of brain arteriovenous malformations. Cerebrovasc. Dis. 31, 338–345 (2011).
Weinsheimer, S. et al. G protein-coupled receptor 124 (GPR124) gene polymorphisms and risk of brain arteriovenous malformation. Transl. Stroke Res. 3, 418–427 (2012).
Chen, H. et al. Polymorphisms of the vascular endothelial growth factor A gene and susceptibility to sporadic brain arteriovenous malformation in a Chinese population. J. Clin. Neurosci. 18, 549–553 (2011).
Zhao, Y. et al. The rs522616 polymorphism in the matrix metalloproteinase-3 (MMP-3) gene is associated with sporadic brain arteriovenous malformation in a Chinese population. J. Clin. Neurosci. 17, 1568–1572 (2010).
Weinsheimer, S. et al. Genome-wide association study of brain arteriovenous malformation patients. Stroke 42, abstr. #W MP85 (2011).
Weinsheimer, S. et al. Common polymorphisms in familial vascular malformation genes do not show association with sporadic brain arteriovenous malformation. Stroke 43, abstr. A3666 (2012).
Sturiale, C. L. et al. Association between the rs1333040 polymorphism on the chromosomal 9p21 locus and sporadic brain arteriovenous malformations. J. Neurol. Neurosurg. Psychiatry 84, 1059–1062 (2013).
Holdt, L. M. & Teupser, D. Recent studies of the human chromosome 9p21 locus, which is associated with atherosclerosis in human populations. Arterioscler. Thromb. Vasc. Biol. 32, 196–206 (2012).
Helgadottir, A. et al. The same sequence variant on 9p21 associates with myocardial infarction, abdominal aortic aneurysm and intracranial aneurysm. Nat. Genet. 40, 217–224 (2008).
Bendjilali, N. et al. Genetic variants on 9p21.3 are associated with brain arteriovenous malformations with associated arterial aneurysms. Stroke 44, abstr. TMP30 (2013).
Emond, M. J. et al. Exome sequencing of extreme phenotypes identifies DCTN4 as a modifier of chronic Pseudomonas aeruginosa infection in cystic fibrosis. Nat. Genet. 44, 886–889 (2012).
Wright, F. A. et al. Genome-wide association and linkage identify modifier loci of lung disease severity in cystic fibrosis at 11p13 and 20q13.2. Nat. Genet. 43, 539–546 (2011).
Drumm, M. L. et al. Genetic modifiers of lung disease in cystic fibrosis. N. Engl. J. Med. 353, 1443–1453 (2005).
Pawlikowska, L. et al. Polymorphisms in genes involved in inflammatory and angiogenic pathways and the risk of hemorrhagic presentation of brain arteriovenous malformations. Stroke 35, 2294–2300 (2004).
Weinsheimer, S. et al. EPHB4 gene polymorphisms and risk of intracranial hemorrhage in patients with brain arteriovenous malformations. Circ. Cardiovasc. Genet. 2, 476–482 (2009).
Pawlikowska, L. et al. Apoliprotein E epsilon2 is associated with new hemorrhage risk in brain arteriovenous malformation. Neurosurgery 58, 838–843; discussion 838–843 (2006).
Achrol, A. S. et al. TNFα-238G>A promoter polymorphism is associated with increased risk of new hemorrhage in the natural course of patients with brain arteriovenous malformations. J. Neurosurg. Anesthesiol. 17, 217–218 (2005).
Sturiale, C. L. et al. Single nucleotide polymorphisms associated with sporadic brain arteriovenous malformations: where do we stand? Brain 136, 665–681 (2013).
Achrol, A. S. et al. Association of tumor necrosis factor-α-238G>A and Apolipoprotein E2 polymorphisms with intracranial hemorrhage after brain arteriovenous malformation treatment. Neurosurgery 61, 731–739; discussion 740 (2007).
McAllister, T. et al. Polymorphisms in the brain derived neurotrophic factor (BDNF) gene influence memory and processing speed one month after brain injury. J. Neurotrauma 29, 1111–1118 (2012).
Qin, L., Kim, E., Ratan, R., Lee, F. S. & Cho, S. Genetic variant of BDNF (Val66Met) polymorphism attenuates stroke-induced angiogenic responses by enhancing anti-angiogenic mediator CD36 expression. J. Neurosci. 31, 775–783 (2011).
Siironen, J. et al. The Met allele of the BDNF Val66Met polymorphism predicts poor outcome among survivors of aneurysmal subarachnoid hemorrhage. Stroke 38, 2858–2860 (2007).
Westbroek, E. M. et al. Brain-derived neurotrophic factor Val66Met polymorphism predicts worse functional outcome after surgery patients with unruptured brain arteriovenous malformation. Stroke 43, 2255–2257 (2012).
Sato, S., Kodama, N., Sasaki, T., Matsumoto, M. & Ishikawa, T. Perinidal dilated capillary networks in cerebral arteriovenous malformations. Neurosurgery 54, 163–168; discussion 168–170 (2004).
Shankar, J. J. et al. Angioarchitecture of brain AVM determines the presentation with seizures: proposed scoring system. AJNR Am. J. Neuroradiol. 34, 1028–1034 (2013).
Geibprasert, S. et al. Hydrocephalus in unruptured brain arteriovenous malformations: pathomechanical considerations, therapeutic implications, and clinical course. J. Neurosurg. 110, 500–507 (2009).
Lasjaunias, P. L. et al. Cerebral proliferative angiopathy: clinical and angiographic description of an entity different from cerebral AVMs. Stroke 39, 878–885 (2008).
Krings, T., Geibprasert, S. & Terbrugge, K. Classification and endovascular management of pediatric cerebral vascular malformations. Neurosurg. Clin. N. Am. 21, 463–482 (2010).
Bharatha, A. et al. Brain arteriovenous malformation multiplicity predicts the diagnosis of hereditary hemorrhagic telangiectasia: quantitative assessment. Stroke 43, 72–78 (2012).
Geibprasert, S. et al. Radiologic assessment of brain arteriovenous malformations: what clinicians need to know. Radiographics 30, 483–501 (2010). This article summarizes the imaging features of brain arteriovenous malformations.
Kim, D. J. & Krings, T. Whole-brain perfusion CT patterns of brain arteriovenous malformations: a pilot study in 18 patients. AJNR Am. J. Neuroradiol. 32, 2061–2066 (2011).
Redekop, G., TerBrugge, K., Montanera, W. & Willinsky, R. Arterial aneurysms associated with cerebral arteriovenous malformations: classification, incidence, and risk of hemorrhage. J. Neurosurg. 89, 539–546 (1998).
Krings, T., Hans, F. J., Geibprasert, S. & Terbrugge, K. Partial “targeted” embolisation of brain arteriovenous malformations. Eur. Radiol. 20, 2723–2731 (2010).
Abla, A. A. et al. Silent arteriovenous malformation hemorrhage and the recognition of “unruptured” arteriovenous malformation patients who benefit from surgical intervention. Neurosurgery 76, 592–600 (2015).
Spetzler, R. F. & Martin, N. A. A proposed grading system for arteriovenous malformations. J. Neurosurg. 65, 476–483 (1986). The grading system proposed in this paper has become an established predictor of risk associated with brain surgery to eliminate arteriovenous malformations. The paper also describes the anatomy of brain arteriovenous malformations.
Kim, H. et al. Evaluating performance of the Spetzler–Martin supplemented model in selecting patients with brain arteriovenous malformation for surgery. Stroke 43, 2497–2499 (2012).
Lawton, M. T., Kim, H., McCulloch, C. E., Mikhak, B. & Young, W. L. A supplementary grading scale for selecting patients with brain arteriovenous malformations for surgery. Neurosurgery 66, 702–713; discussion 713 (2010). The grading system proposed in this paper increased the predictive accuracy of the Spetzler–Martin grading system and has become an important tool for selecting patients for surgery.
Kim, H. et al. Validation of the supplemented Spetzler–Martin grading system for brain arteriovenous malformations in a multicenter cohort of 1009 surgical patients. Neurosurgery 76, 25–33 (2015). This study validated the Lawton–Young grading system in a multicentre cohort of more than 1,000 patients, demonstrating that methods to select patients for surgery are evolving and improving.
Lawton, M. Seven AVMs: Tenets and Techniques for Resection. xiii–xiv (Thieme Medical Publishers, 2014).
Davidson, A. S. & Morgan, M. K. How safe is arteriovenous malformation surgery? A prospective, observational study of surgery as first-line treatment for brain arteriovenous malformations. Neurosurgery 66, 498–504; discussion 504–505 (2010).
Hamilton, M. G. & Spetzler, R. F. The prospective application of a grading system for arteriovenous malformations. Neurosurgery 34, 2–6; discussion 6–7 (1994).
Hartmann, A. et al. Determinants of neurological outcome after surgery for brain arteriovenous malformation. Stroke 31, 2361–2364 (2000).
Heros, R. C., Korosue, K. & Diebold, P. M. Surgical excision of cerebral arteriovenous malformations: late results. Neurosurgery 26, 570–577; discussion 577–578 (1990).
Morgan, M. K., Rochford, A. M., Tsahtsarlis, A., Little, N. & Faulder, K. C. Surgical risks associated with the management of grade I and II brain arteriovenous malformations. Neurosurgery 54, 832–837; discussion 837–839 (2004).
Pikus, H. J., Beach, M. L. & Harbaugh, R. E. Microsurgical treatment of arteriovenous malformations: analysis and comparison with stereotactic radiosurgery. J. Neurosurg. 88, 641–646 (1998).
Schaller, C. & Schramm, J. Microsurgical results for small arteriovenous malformations accessible for radiosurgical or embolization treatment. Neurosurgery 40, 664–672; discussion 672–674 (1997).
Schaller, C., Schramm, J. & Haun, D. Significance of factors contributing to surgical complications and to late outcome after elective surgery of cerebral arteriovenous malformations. J. Neurol. Neurosurg. Psychiatry 65, 547–554 (1998).
Sisti, M. B., Kader, A. & Stein, B. M. Microsurgery for 67 intracranial arteriovenous malformations less than 3 cm in diameter. J. Neurosurg. 79, 653–660 (1993).
Sundt, T. M. Jr, Piepgras, D. G. & Stevens, L. N. Surgery for supratentorial arteriovenous malformations. Clin. Neurosurg. 37, 49–115 (1991).
Potts, M. B. et al. Current surgical results with low-grade brain arteriovenous malformations. J. Neurosurg. 122, 912–920 (2015). This article summarizes current opinion on the role of surgery in the treatment of brain arteriovenous malformations.
Valavanis, A. & Yasargil, M. G. The endovascular treatment of brain arteriovenous malformations. Adv. Tech. Stand. Neurosurg. 24, 131–214 (1998).
Yu, S. C., Chan, M. S., Lam, J. M., Tam, P. H. & Poon, W. S. Complete obliteration of intracranial arteriovenous malformation with endovascular cyanoacrylate embolization: initial success and rate of permanent cure. AJNR Am. J. Neuroradiol. 25, 1139–1143 (2004).
Katsaridis, V., Papagiannaki, C. & Aimar, E. Curative embolization of cerebral arteriovenous malformations (AVMs) with Onyx in 101 patients. Neuroradiology 50, 589–597 (2008).
Taylor, C. L. et al. Complications of preoperative embolization of cerebral arteriovenous malformations. J. Neurosurg. 100, 810–812 (2004).
Meisel, H. J. et al. Effect of partial targeted N-butyl-cyano-acrylate embolization in brain AVM. Acta Neurochir. 144, 879–887; discussion 888 (2002).
da Costa, L. et al. The natural history and predictive features of hemorrhage from brain arteriovenous malformations. Stroke 40, 100–105 (2009).
Karlsson, B., Lindquist, C. & Steiner, L. Prediction of obliteration after Gamma Knife surgery for cerebral arteriovenous malformations. Neurosurgery 40, 425–430; discussion 430–431 (1997).
Kemeny, A. A., Dias, P. S. & Forster, D. M. Results of stereotactic radiosurgery of arteriovenous malformations: an analysis of 52 cases. J. Neurol. Neurosurg. Psychiatry 52, 554–558 (1989).
Lunsford, L. D. et al. Stereotactic radiosurgery for arteriovenous malformations of the brain. J. Neurosurg. 75, 512–524 (1991).
Dwenger, A., Funck, M., Lueken, B., Schweitzer, G. & Lehmann, U. Effect of ascorbic acid on neutrophil functions and hypoxanthine/xanthine oxidase-generated, oxygen-derived radicals. Eur. J. Clin. Chem. Clin. Biochem. 30, 187–191 (1992).
Steiner, L. et al. Clinical outcome of radiosurgery for cerebral arteriovenous malformations. J. Neurosurg. 77, 1–8 (1992).
Yamamoto, M., Jimbo, M., Hara, M., Saito, I. & Mori, K. Gamma Knife radiosurgery for arteriovenous malformations: long-term follow-up results focusing on complications occurring more than 5 years after irradiation. Neurosurgery 38, 906–914 (1996).
Yamamoto, M. et al. Long-term follow-up of radiosurgically treated arteriovenous malformations in children: report of nine cases. Surg. Neurol. 38, 95–100 (1992).
Yamamoto, M. et al. Long-term results of radiosurgery for arteriovenous malformation: neurodiagnostic imaging and histological studies of angiographically confirmed nidus obliteration. Surg. Neurol. 37, 219–230 (1992).
Monaco, E. A. et al. Management of adverse radiation effects after radiosurgery for arteriovenous malformations. Prog. Neurol. Surg. 27, 107–118 (2013).
Kano, H. et al. Stereotactic radiosurgery for arteriovenous malformations, Part 3: outcome predictors and risks after repeat radiosurgery. J. Neurosurg. 116, 21–32 (2012).
Kano, H. et al. Stereotactic radiosurgery for arteriovenous malformations, Part 1: management of Spetzler–Martin grade I and II arteriovenous malformations. J. Neurosurg. 116, 11–20 (2012).
Plasencia, A. R. & Santillan, A. Embolization and radiosurgery for arteriovenous malformations. Surg. Neurol. Int. 3, S90–S104 (2012).
Pollock, B. E., Flickinger, J. C., Lunsford, L. D., Maitz, A. & Kondziolka, D. Factors associated with successful arteriovenous malformation radiosurgery. Neurosurgery 42, 1239–1244; discussion 1244–1247 (1998). This article demonstrates that analyses of radiosurgical results lead to predictors of outcome and grading systems that guide clinical decision-making.
Shin, M. et al. Analysis of nidus obliteration rates after Gamma Knife surgery for arteriovenous malformations based on long-term follow-up data: the University of Tokyo experience. J. Neurosurg. 101, 18–24 (2004).
Aoyama, H. et al. Treatment outcome of single or hypofractionated single-isocentric stereotactic irradiation (STI) using a linear accelerator for intracranial arteriovenous malformation. Radiother. Oncol. 59, 323–328 (2001).
Hadjipanayis, C. G. et al. Stereotactic radiosurgery for motor cortex region arteriovenous malformations. Neurosurgery 48, 70–76; discussion 76–77 (2001).
Nakamura, J. L. et al. Dose conformity of Gamma Knife radiosurgery and risk factors for complications. Int. J. Radiat. Oncol. Biol. Phys. 51, 1313–1319 (2001).
Levegrun, S., Hof, H., Essig, M., Schlegel, W. & Debus, J. Radiation-induced changes of brain tissue after radiosurgery in patients with arteriovenous malformations: dose/volume-response relations. Strahlenther. Onkol. 180, 758–767 (2004).
Pollock, B. E., Gorman, D. A. & Brown, P. D. Radiosurgery for arteriovenous malformations of the basal ganglia, thalamus, and brainstem. J. Neurosurg. 100, 210–214 (2004).
Inoue, H. K. Long-term results of gamma knife surgery for arteriovenous malformations: 10- to 15-year follow up in patients treated with lower doses. J. Neurosurg. 105 (Suppl.), 64–68 (2006).
Sirin, S. et al. Prospective staged volume radiosurgery for large arteriovenous malformations: indications and outcomes in otherwise untreatable patients. Neurosurgery 58, 17–27; discussion 17–27 (2006).
Liscak, R. et al. Arteriovenous malformations after Leksell Gamma Knife radiosurgery: rate of obliteration and complications. Neurosurgery 60, 1005–1014; discussion 1015–1016 (2007).
Ganz, J. C., Reda, W. A. & Abdelkarim, K. Adverse radiation effects after Gamma Knife surgery in relation to dose and volume. Acta Neurochir. 151, 9–19 (2009).
Lunsford, L. D., Niranjan, A., Kano, H. & Kondziolka, D. The technical evolution of Gamma Knife radiosurgery for arteriovenous malformations. Prog. Neurol. Surg. 27, 22–34 (2013).
Huang, P. P. et al. Long-term outcomes after staged-volume stereotactic radiosurgery for large arteriovenous malformations. Neurosurgery 71, 632–643; discussion 643–644 (2012).
Barker, F. G. et al. Dose-volume prediction of radiation-related complications after proton beam radiosurgery for cerebral arteriovenous malformations. J. Neurosurg. 99, 254–263 (2003).
Kjellberg, R. N., Hanamura, T., Davis, K. R., Lyons, S. L. & Adams, R. D. Bragg-peak proton-beam therapy for arteriovenous malformations of the brain. N. Engl. J. Med. 309, 269–274 (1983).
Pollock, B. E., Kondziolka, D., Lunsford, L. D., Bissonette, D. & Flickinger, J. C. Repeat stereotactic radiosurgery of arteriovenous malformations: factors associated with incomplete obliteration. Neurosurgery 38, 318–324 (1996).
Flickinger, J. C. An integrated logistic formula for prediction of complications from radiosurgery. Int. J. Radiat. Oncol. Biol. Phys. 17, 879–885 (1989).
Kano, H. et al. Stereotactic radiosurgery for arteriovenous malformations, Part 6: multistaged volumetric management of large arteriovenous malformations. J. Neurosurg. 116, 54–65 (2012).
Zhang, X. Q. et al. Clinical significance of 3D reconstruction of arteriovenous malformation using digital subtraction angiography and its modification with CT information in stereotactic radiosurgery. Int. J. Radiat. Oncol. Biol. Phys. 57, 1392–1399 (2003).
Maitz, A. H. et al. Tube angulation improves angiographic targeting of arteriovenous malformations during stereotactic radiosurgery. Comput. Aided Surg. 6, 225–229 (2001).
Bednarz, G., Downes, B., Werner-Wasik, M. & Rosenwasser, R. H. Combining stereotactic angiography and 3D time-of-flight magnetic resonance angiography in treatment planning for arteriovenous malformation radiosurgery. Int. J. Radiat. Oncol. Biol. Phys. 46, 1149–1154 (2000).
Colombo, F. et al. Three-dimensional angiography for radiosurgical treatment planning for arteriovenous malformations. J. Neurosurg. 98, 536–543 (2003).
Hamm, K. D. et al. Special aspects of diagnostic imaging for radiosurgery of arteriovenous malformations. Neurosurgery 62, A44–A52; discussion A52 (2008).
Flickinger, J. C., Kano, H., Niranjan, A., Kondziolka, D. & Lunsford, L. D. Dose selection in stereotactic radiosurgery. Prog. Neurol. Surg. 27, 49–57 (2013).
Boothe, D. et al. Bevacizumab as a treatment for radiation necrosis of brain metastases post stereotactic radiosurgery. Neuro Oncol. 15, 1257–1263 (2013).
Alexander, M. J. & Tolbert, M. E. Targeting cerebral arteriovenous malformations for minimally invasive therapy. Neurosurgery 59, S178–183; discussion S3–S13 (2006).
Bollet, M. A. et al. Efficacy and morbidity of arc-therapy radiosurgery for cerebral arteriovenous malformations: a comparison with the natural history. Int. J. Radiat. Oncol. Biol. Phys. 58, 1353–1363 (2004).
Chang, S. D. et al. Multimodality treatment of giant intracranial arteriovenous malformations. Neurosurgery 53, 1–11; discussion 11–13 (2003).
Dawson, R. C. et al. Treatment of arteriovenous malformations of the brain with combined embolization and stereotactic radiosurgery: results after 1 and 2 years. AJNR Am. J. Neuroradiol. 11, 857–864 (1990).
Deruty, R., Pelissou-Guyotat, I., Morel, C., Bascoulergue, Y. & Turjman, F. Reflections on the management of cerebral arteriovenous malformations. Surg. Neurol. 50, 245–255; discussion 255–256 (1998).
Deruty, R., Pelissou-Guyotat, I., Mottolese, C., Bascoulergue, Y. & Amat, D. The combined management of cerebral arteriovenous malformations. Experience with 100 cases and review of the literature. Acta Neurochir. 123, 101–112 (1993).
Fiorella, D., Albuquerque, F. C., Woo, H. H., McDougall, C. G. & Rasmussen, P. A. The role of neuroendovascular therapy for the treatment of brain arteriovenous malformations. Neurosurgery 59, S163–S177; discussion S3–13 (2006).
Gobin, Y. P. et al. Treatment of brain arteriovenous malformations by embolization and radiosurgery. J. Neurosurg. 85, 19–28 (1996).
Guo, W. Y. et al. Combined embolization and Gamma Knife radiosurgery for cerebral arteriovenous malformations. Acta Radiol. 34, 600–606 (1993).
Haw, C. S., terBrugge, K., Willinsky, R. & Tomlinson, G. Complications of embolization of arteriovenous malformations of the brain. J. Neurosurg. 104, 226–232 (2006).
Henkes, H. et al. Endovascular therapy of brain AVMs prior to radiosurgery. Neurol. Res. 20, 479–492 (1998).
Killer, M. et al. Radiosurgery following embolisation and/or surgery of brain AVM's. Interv. Neuroradiol. 2, 27–33 (1996).
Mathis, J. A. et al. The efficacy of particulate embolization combined with stereotactic radiosurgery for treatment of large arteriovenous malformations of the brain. AJNR Am. J. Neuroradiol. 16, 299–306 (1995).
Miyachi, S. et al. Embolization of arteriovenous malformations prior to radiosurgery. Interv. Neuroradiol. 6 (Suppl. 1), 131–137 (2000).
Mizoi, K. et al. Multimodality treatment for large and critically located arteriovenous malformations. Neurol. Med. Chir. 38 (Suppl.), 186–192 (1998).
Soderman, M., Andersson, T., Karlsson, B., Wallace, M. C. & Edner, G. Management of patients with brain arteriovenous malformations. Eur. J. Radiol. 46, 195–205 (2003).
Soderman, M., Rodesch, G., Karlsson, B., Lax, I. & Lasjaunias, P. Gamma Knife outcome models as a reference standard in the embolisation of cerebral arteriovenous malformations. Acta Neurochir. 143, 801–810 (2001).
Wikholm, G., Lundqvist, C. & Svendsen, P. The Goteborg cohort of embolized cerebral arteriovenous malformations: a 6-year follow-up. Neurosurgery 49, 799–805; discussion 805–806 (2001).
Andrade-Souza, Y. M. et al. Embolization before radiosurgery reduces the obliteration rate of arteriovenous malformations. Neurosurgery 60, 443–451; discussion 451–452 (2007).
Back, A. G., Vollmer, D., Zeck, O., Shkedy, C. & Shedden, P. M. Retrospective analysis of unstaged and staged Gamma Knife surgery with and without preceding embolization for the treatment of arteriovenous malformations. J. Neurosurg. 109 (Suppl.), 57–64 (2008).
Kano, H. et al. Stereotactic radiosurgery for arteriovenous malformations after embolization: a case–control study. J. Neurosurg. 117, 265–275 (2012).
Miyawaki, L. et al. Five year results of LINAC radiosurgery for arteriovenous malformations: outcome for large AVMS. Int. J. Radiat. Oncol. Biol. Phys. 44, 1089–1106 (1999).
Ogilvy, C. S. et al. AHA Scientific Statement: recommendations for the management of intracranial arteriovenous malformations: a statement for healthcare professionals from a special writing group of the Stroke Council, American Stroke Association. Stroke 32, 1458–1471 (2001). This article summarizes management recommendations for brain arteriovenous malformations from a panel of experts.
Pan, H. C., Sheehan, J., Stroila, M., Steiner, M. & Steiner, L. Late cyst formation following Gamma Knife surgery of arteriovenous malformations. J. Neurosurg. 102 (Suppl.), 124–127 (2005).
Paulsen, R. D., Steinberg, G. K., Norbash, A. M., Marcellus, M. L. & Marks, M. P. Embolization of basal ganglia and thalamic arteriovenous malformations. Neurosurgery 44, 991–996; discussion 996–997 (1999).
Sinclair, J., Kelly, M. E. & Steinberg, G. K. Surgical management of posterior fossa arteriovenous malformations. Neurosurgery 58 (Suppl. 2), ONS-189–201; discussion ONS–201 (2006).
Andrade-Souza, Y. M. et al. Liquid embolisation material reduces the delivered radiation dose: a physical experiment. Acta Neurochir. 150, 161–164; discussion 164 (2008).
Miyamoto, S. et al. Posttreatment sequelae of palliatively treated cerebral arteriovenous malformations. Neurosurgery 46, 589–594; discussion 594–595 (2000).
Morgan, M. K., Patel, N. J., Simons, M., Ritson, E. A. & Heller, G. Z. Influence of the combination of patient age and deep venous drainage on brain arteriovenous malformation recurrence after surgery. J. Neurosurg. 117, 934–941 (2012).
Abla, A. A. et al. A treatment paradigm for high-grade brain arteriovenous malformations: volume-staged radiosurgical downgrading followed by microsurgical resection. J. Neurosurg. 122, 419–432 (2015).
Rutledge, W. C. et al. Treatment and outcomes of ARUBA-eligible patients with unruptured brain arteriovenous malformations at a single institution. Neurosurg. Focus 37, E8 (2014).
Stapf, C., Parides, M. K., Moskowitz, A. J. & Mohr, J. P. Management of brain arteriovenous malformations — authors’ reply. Lancet 383, 1635–1636 (2014).
Han, P. P., Ponce, F. A. & Spetzler, R. F. Intention-to-treat analysis of Spetzler–Martin grades IV and V arteriovenous malformations: natural history and treatment paradigm. J. Neurosurg. 98, 3–7 (2003).
Dorman, P. J., Slattery, J., Farrell, B., Dennis, M. S. & Sandercock, P. A. A randomised comparison of the EuroQol and Short Form-36 after stroke. United Kingdom Collaborators in the International Stroke Trial. BMJ 315, 461 (1997).
Marshall, G. A., Jonker, B. P., Morgan, M. K. & Taylor, A. J. Prospective study of neuropsychological and psychosocial outcome following surgical excision of intracerebral arteriovenous malformations. J. Clin. Neurosci. 10, 42–47 (2003).
Brown, R. D. Jr et al. The natural history of unruptured intracranial arteriovenous malformations. J. Neurosurg. 68, 352–357 (1988).
Gross, B. A. & Du, R. Natural history of cerebral arteriovenous malformations: a meta-analysis. J. Neurosurg. 118, 437–443 (2013). References 189 and 190 provide reviews of the natural history of brain arteriovenous malformations.
Bervini, D., Morgan, M. K., Ritson, E. A. & Heller, G. Surgery for unruptured arteriovenous malformations of the brain is better than conservative management for selected cases: a prospective cohort study. J. Neurosurg. 121, 878–890 (2014).
Choi, J. H. et al. Clinical outcome after first and recurrent hemorrhage in patients with untreated brain arteriovenous malformation. Stroke 37, 1243–1247 (2006).
Baranoski, J. F. et al. Seizure control for intracranial arteriovenous malformations is directly related to treatment modality: a meta-analysis. J. Neurointerv. Surg. 6, 684–690 (2014).
Thorpe, M. L., Cordato, D. J., Morgan, M. K. & Herkes, G. K. Postoperative seizure outcome in a series of 114 patients with supratentorial arteriovenous malformations. J. Clin. Neurosci. 7, 107–111 (2000).
van Beijnum, J. et al. Treatment of brain arteriovenous malformations: a systematic review and meta-analysis. JAMA 306, 2011–2019 (2011). This meta-analysis compiled data comparing the morbidity, mortality and efficacy of surgery, radiosurgery and endovascular embolization in more than 13,000 patients.
Gross, B. A. & Du, R. Hemorrhage from arteriovenous malformations during pregnancy. Neurosurgery 71, 349–355; discussion 355–356 (2012).
Bateman, B. T. et al. Intracerebral hemorrhage in pregnancy: frequency, risk factors, and outcome. Neurology 67, 424–429 (2006).
Horton, J. C., Chambers, W. A., Lyons, S. L., Adams, R. D. & Kjellberg, R. N. Pregnancy and the risk of hemorrhage from cerebral arteriovenous malformations. Neurosurgery 27, 867–871; discussion 871–872 (1990).
Lawton, M. T. et al. Radiation arteriopathy in the transgenic arteriovenous fistula model. Neurosurgery 62, 1129–1138; discussion 138–139 (2008).
Walker, E. J. et al. Arteriovenous malformation in the adult mouse brain resembling the human disease. Ann. Neurol. 69, 954–962 (2011). This experimental model for brain arteriovenous malformations was the first of its kind and provided a method for the pathogenesis and regression of this condition.
Han, C. et al. VEGF neutralization can prevent and normalize arteriovenous malformations in an animal model for hereditary hemorrhagic telangiectasia 2. Angiogenesis 14, 823–830 (2014).
Frenzel, T. et al. Feasibility of minocycline and doxycycline use as potential vasculostatic therapy for brain vascular malformations: pilot study of adverse events and tolerance. Cerebrovasc. Dis. 25, 157–163 (2008). This study demonstrated that brain arteriovenous malformations might be stabilized and haemorrhage rates reduced with medical therapy.
Hashimoto, T., Matsumoto, M. M., Li, J. F., Lawton, M. T. & Young, W. L. Suppression of MMP-9 by doxycycline in brain arteriovenous malformations. BMC Neurol. 5, 1 (2005).
Feliciano, C. E. et al. Provocative test with propofol: experience in patients with cerebral arteriovenous malformations who underwent neuroendovascular procedures. AJNR Am. J. Neuroradiol. 31, 470–475 (2010).
Starke, R. M. et al. Adjuvant embolization with N-butyl cyanoacrylate in the treatment of cerebral arteriovenous malformations: outcomes, complications, and predictors of neurologic deficits. Stroke 40, 2783–2790 (2009).
Mann, K. M. et al. Sleeping Beauty mutagenesis reveals cooperating mutations and pathways in pancreatic adenocarcinoma. Proc. Natl Acad. Sci. USA 109, 5934–5941 (2012).
O'Hayre, M. et al. The emerging mutational landscape of G proteins and G-protein-coupled receptors in cancer. Nat. Rev. Cancer 13, 412–424 (2013).
Forbes, S. A. et al. COSMIC: mining complete cancer genomes in the Catalogue of Somatic Mutations in Cancer. Nucleic Acids Res. 39, D945–D950 (2011).
Lawton, M. T. The role of AVM microsurgery in the aftermath of a randomized trial of unruptured brain arteriovenous malformations. AJNR Am. J. Neuroradiol. 36, 617–619 (2015).
Acknowledgements
This primer cites research that was supported in part by US National Institutes of Health grants: R01 NS034949 (H.K.) and U54 NS065075 (M.T.L.). The Brain Vascular Malformation Consortium (U54NS065075) is part of the Rare Diseases Clinical Research Network (RDCRN), an initiative of the Office of Rare Diseases Research (ORDR) that is funded through collaboration between National Center for Advancing Translational Sciences (NCATS) and the National Institute of Neurological Disorders and Stroke (NINDS).
Author information
Authors and Affiliations
Contributions
Introduction (M.T.L.); Epidemiology (W.C.R., H.K. and C.S.); Mechanisms/pathophysiology (K.J.W., D.Y.L. and H.K.); Diagnosis, screening and prevention (T.K. and K.T.B.); Management (M.T.L., T.K., K.T.B. and D.K.); Quality of life (M.K.M.); Outlook (K.M., R.F.S., M.T.L. and H.K.); overview of Primer (M.T.L.).
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Lawton, M., Rutledge, W., Kim, H. et al. Brain arteriovenous malformations. Nat Rev Dis Primers 1, 15008 (2015). https://doi.org/10.1038/nrdp.2015.8
Published:
DOI: https://doi.org/10.1038/nrdp.2015.8
This article is cited by
-
Postsurgical dural supply to the spinal cord arteriovenous malformation in spinal arteriovenous metameric syndrome
Neuroradiology (2023)
-
Localized conditional induction of brain arteriovenous malformations in a mouse model of hereditary hemorrhagic telangiectasia
Angiogenesis (2023)
-
Understanding the pathogenesis of brain arteriovenous malformation: genetic variations, epigenetics, signaling pathways, and immune inflammation
Human Genetics (2023)
-
Application of diffusion tensor-based tractography in treatment of brain arteriovenous malformations: a systematic review
Neurosurgical Review (2023)
-
Value of contrast-enhanced MR angiography for the follow-up of treated brain arteriovenous malformations: systematic review and meta-analysis
European Radiology (2023)