Abstract
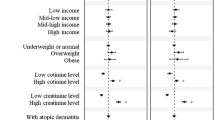
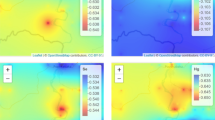
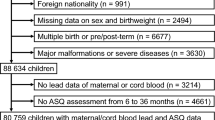
Lead (Pb) has adverse effects on our nervous system and renal systems. Young children are more vulnerable to Pb exposure. However, the role of low-level Pb exposure in the immune system and allergic diseases in children is not well established. The aims of this study are to investigate the associations between Pb exposure and allergic diseases; between Pb and immunoglobulin E (IgE) as an intervening variable; and gender-based differences. We used multistage stratified random sampling to recruit kindergarten children nationwide in Taiwan. Information about allergic diseases and environmental exposures was collected by questionnaire. We compared children with and without allergic diseases for blood Pb levels measured by inductively coupled plasma mass spectrometry. The association between blood Pb and allergic diseases was assessed by logistic regression and those between Pb and IgE by generalized linear models. We also conducted mediation analysis to evaluate how much risk of allergic diseases related to Pb exposure is explained by IgE. A total of 930 children completed specimen collections. There was a positive association between Pb and asthma. Blood Pb were also positively linked with serum IgE (β=0.26 kU/l per ln-unit increase Pb concentration; 95% CI 0.009–0.50 kU/l), after adjusting for potential confounders. Analyses stratified by gender revealed that blood Pb correlated with IgE only in boys (β=0.40 kU/l; 95% CI 0.03–0.76 kU/l). We estimated that 38% of the total effect of Pb exposure on asthma is mediated by IgE levels. In conclusion, Pb exposure is associated with both blood IgE and asthma in boys. Moreover, the effect of Pb exposure on asthma may be mediated by IgE levels.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Yang SN, Hsieh CC, Kuo HF, Lee MS, Huang MY, Kuo CH et al. The effects of environmental toxins on allergic inflammation. Allergy Asthma Immunol Res 2014; 6: 478–484.
Annesi-Maesano I, Pollitt R, King G, Bousquet J, Hellier G, Sahuquillo J et al. In utero exposure to lead and cord blood total IgG. Is there a connection? Allergy 2003; 58: 589–594.
Roberts A . Lead Poisoning: The Truth Behind Consumer Products and Legislation 2010: available at https://www.lead.org.au/Lead_Poisoning_The_Truth_Behind_Consumer_Products_and_Legislation.pdf. (accessed 11 August 2016).
Min JY, Min KB, Kim R, Cho SI, Paek D . Blood lead levels and increased bronchial responsiveness. Biol Trace Elem Res 2008; 123: 41–46.
U.S. Department of Health and Human Services. Toxicological Profile for Lead (update) Public Health Service Agency for Toxic Substances and Disease Registry, 2007, available at http://www.atsdr.cdc.gov/toxprofiles/tp13.pdf. (accessed 15 August 2016).
China Post. More Lead-Based Pipes Revealed in Greater Taipei 2015: available at http://www.chinapost.com.tw/taiwan/national/national-news/2015/10/23/449046/More-lead-based.htm. (accessed 15 August 2016).
Lo A . Explainer: How the Water Lead Contamination Scare Became a Citywide Concern. Hong Kong Free Press. 2015. https://www.hongkongfp.com/2015/07/13/explainer-how-a-public-estates-lead-contamination-became-a-ciytwide-concern/ (accessed 25 August 2016).
Mcwhirter C, Maher K . Flint water crisis shines light on lead pipes across U.S. Wall Street J2016. https://www.wsj.com/articles/flint-water-crisis-shines-light-on-lead-pipes-crisscrossing-the-us-1453977180 (accessed 30 August 2016).
Gidlow DA . Lead toxicity. Occup Med (Lond) 2015; 65: 348–356.
Heo Y, Lee BK, Ahn KD, Lawrence DA . Serum IgE elevation correlates with blood lead levels in battery manufacturing workers. Hum ExpToxicol 2004; 23: 209–213.
Hwang YH, Lin YS, Lin CY, Wang IJ . Incense burning at home and the blood lead level of preschoolers in Taiwan. Environ Sci Pollut Res Int 2014; 21: 13480–13487.
Soto-Martínez ME, Avila L, Soto-Quirós ME . New criteria for the diagnosis and management of asthma in children under 5 years old: GINA guidelines An. An Pediatr (Barc) 2009; 71: 91–94.
Barany E, Bergdahl IA, Schutz A, Skerfving S, Oskarsson A . Inductively coupled plasma mass spectrometry for direct multi-element analysis of diluted human blood and serum. J Anal At Spectrom 1997; 12: 1005–1009.
Needleman HL, Landrigan PJ . What level of lead in blood is toxic for a child? Am J Public Health 2004; 94: 8.
Surkan PJ, Zhang A, Trachtenberg F, Daniel DB, McKinlay S, Bellinger DC . Neuropsychological function in children with blood lead levels <10 microg/dl. Neurotoxicology 2007; 28: 1170–1177.
Ditlevsen S, Christensen U, Lynch J, Damsgaard MT, Keiding N . The mediation proportion: a structural equation approach for estimating the proportion of exposure effect on outcome explained by an intermediate variable. Epidemiology 2005; 16: 114–120.
CDC. What Do Parents Need to Know to Protect Their Children? 2012: available at https://www.cdc.gov/nceh/lead/acclpp/blood_lead_levels.htm. (accepted 7 February 2017).
Farkhondeh T, Boskabady MH, Jalali S, Bayrami G . The effect of lead exposure on tracheal responsiveness to methacholine and ovalbumin, total and differential white blood cells count, and serum levels of immunoglobulin E, histamine, and cytokines in guinea pigs. Hum ExpToxicol 2014; 33: 325–333.
Min KB, Min JY . Environmental lead exposure and increased risk for total and allergen-specific IgE in US adults. J Allergy Clin Immunol 2015; 135: 275–277.
Karmaus W, Brooks KR, Nebe T, Witten J, Obi-Osius N, Kruse H . Immune function biomarkers in children exposed to lead and organochlorine compounds: a cross-sectional study. Environ Health 2005; 4: 5.
Pugh Smith P, Nriagu JO . Lead poisoning and asthma among low-income and African American children in Saginaw, Michigan. Environ Res 2011; 111: 81–86.
Mohammed AA, Mohamed FY, El-Okda EL-S, Ahmed AB . Blood lead levels and childhood asthma. Indian Pediatr 2015; 52: 303–306.
Park S, Lee EH, Kho Y . The association of asthma, total IgE, and blood lead and cadmium levels. J Allergy Clin Immunol 2016; 138: 1701–1703.e6.
Myers SN, Rowell B, Binns HJ . Lead poisoning and asthma: an examination of comorbidity. Arch PediatrAdolesc Med 2002; 156: 863–866.
Mener DJ, Garcia-Esquinas E, Navas-Acien A, Dietert RR, Shargorodsky J, Lin SY . Lead exposure and increased food allergic sensitization in U.S. children and adults. Int Forum Allergy Rhinol 2015; 5: 214–220.
Wells EM, Bonfield TL, Dearborn DG, Jackson LW . The relationship of blood lead with immunoglobulin E, eosinophils, and asthma among children: NHANES2005-2006. Int J Hyg Environ Health 2014; 217: 196–204.
Oettgen HC, Geha RS . IgE in asthma and atopy: cellular and molecular connections. J Clin Invest 1999; 104: 829–835.
Joseph CL, Havstad S, Ownby DR, Peterson EL, Maliarik M, McCabe MJ, Jr et al. Blood lead level and risk of asthma. Environ Health Perspect 2005; 113: 900–904.
Boskabaddy MH, Farkhondeh T . Inhaled lead exposure affects tracheal responsiveness and lung inflammation in guinea pigs during sensitization. Biol Trace Elem Res 2013; 154: 363–371.
Sen A, Heredia N, Senut MC, Land S, Hollocher K, Lu X et al. Multigenerational epigenetic inheritance in humans: DNA methylation changes associated with maternal exposure to lead can be transmitted to the grandchildren. Sci Rep 2015; 5: 14466.
Sun LI, Hu J, Zhao Z, Li L, Cheng H . Influence of exposure to environmental lead on serum immunoglobulin in preschool children. Environ Res 2003; 92: 124–128.
Statistics Canada. Blood lead concentrations in Canadians, 2009 to 2011 2015: available at http://www.statcan.gc.ca/pub/82-625-x/2013001/article/11779-eng.htm. (accessed 15 August 2016).
Counter SA, Buchanan LH, Ortega F . Gender differences in blood lead and hemoglobin levels in Andean adults with chronic lead exposure. Int J Occup Environ Health 2001; 7: 113–118.
Chi YW, Chen SL, Yang MH, Hwang RC, Chu ML . Heavy metals in traditional Chinese medicine: ba-pao-neu-hwang-san. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi 1993; 34: 181–190.
Griffin TB, Couiston F, Wills H . Biological and clinical effects of continuous exposure to airborne particulate lead. Arh Hig Toksikol 1975; 26: 191–208.
Rabinowitz MB, Wetherill GW, Kopple JD . Kinetic analysis of lead metabolism in healthy humans. J Clin Invest 1976; 58: 260–270.
Acknowledgements
This study was supported by a grant from the Ministry of Science and Technology in Taiwan (MOST 105-2314-B-192-001). We thank Professor Yau-Huei Hwang, Miss Yi-Hseun Lin, and our colleagues for the data collection.
Author contributions
Conception and design, data analysis and interpretation, and manuscript writing: IJW. Interpretation and revisions of the manuscript: WJJK and CCY. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Journal of Exposure Science and Environmental Epidemiology website
Supplementary information
Rights and permissions
About this article
Cite this article
Wang, IJ., Karmaus, W. & Yang, CC. Lead exposure, IgE, and the risk of asthma in children. J Expo Sci Environ Epidemiol 27, 478–483 (2017). https://doi.org/10.1038/jes.2017.5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jes.2017.5
Keywords
This article is cited by
-
Assessment of house dust trace elements and human exposure in Ankara, Turkey
Environmental Science and Pollution Research (2023)
-
Exposure to Heavy Metals and Allergic Outcomes in Children: a Systematic Review and Meta-analysis
Biological Trace Element Research (2022)
-
Evaluation of blood and tooth element status in asthma cases: a preliminary case–control study
BMC Pulmonary Medicine (2021)
-
Maternal metal concentration during gestation and pediatric morbidity in children: an exploratory analysis
Environmental Health and Preventive Medicine (2021)
-
Early life blood lead levels and asthma diagnosis at age 4–6 years
Environmental Health and Preventive Medicine (2021)