Abstract
Malaria is caused in humans by five species of single-celled eukaryotic Plasmodium parasites (mainly Plasmodium falciparum and Plasmodium vivax) that are transmitted by the bite of Anopheles spp. mosquitoes. Malaria remains one of the most serious infectious diseases; it threatens nearly half of the world's population and led to hundreds of thousands of deaths in 2015, predominantly among children in Africa. Malaria is managed through a combination of vector control approaches (such as insecticide spraying and the use of insecticide-treated bed nets) and drugs for both treatment and prevention. The widespread use of artemisinin-based combination therapies has contributed to substantial declines in the number of malaria-related deaths; however, the emergence of drug resistance threatens to reverse this progress. Advances in our understanding of the underlying molecular basis of pathogenesis have fuelled the development of new diagnostics, drugs and insecticides. Several new combination therapies are in clinical development that have efficacy against drug-resistant parasites and the potential to be used in single-dose regimens to improve compliance. This ambitious programme to eliminate malaria also includes new approaches that could yield malaria vaccines or novel vector control strategies. However, despite these achievements, a well-coordinated global effort on multiple fronts is needed if malaria elimination is to be achieved.
Similar content being viewed by others
Introduction
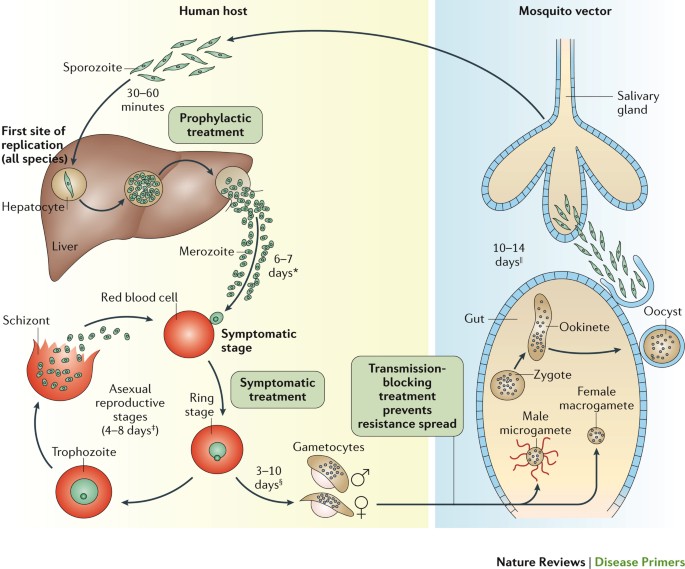
Malaria has had a profound effect on human lives for thousands of years and remains one of the most serious, life-threatening infectious diseases1–3. The disease is caused by protozoan pathogens of the Plasmodium spp.; Plasmodium falciparum and Plasmodium vivax, for which humans are the exclusive mammalian hosts, are the most common species and are responsible for the largest public health burden. Malaria is transmitted by the bite of Plasmodium spp.-infected female mosquitoes of the Anopheles genus1–3. During a blood meal, infected mosquitoes inject — along with their anticoagulating saliva — sporozoites, which are the infective, motile stage of Plasmodium spp. Sporozoites journey through the skin to the lymphatics and into hepatocytes in the liver (Fig. 1). Inside the hepatocyte, a single sporozoite can generate tens of thousands of merozoites (the stage that results from multiple asexual fissions (schizogony) of a sporozoite within the body of the host), which are released into the bloodstream where they enter red blood cells to replicate (erythrocytic schizogony). A fraction of merozoites (those that are sexually committed) also differentiate and mature into male and female gametocytes, which is the stage that infects the mosquito host when it takes a blood meal4,5. The onset of clinical symptoms generally occurs 7–10 days after the initial mosquito bite. P. vivax and Plasmodium ovale also have dormant forms, called hypnozoites, which can emerge from the liver years after the initial infection6, leading to relapse if not treated properly.
The mosquito vector transmits the Plasmodium spp. parasite in the sporozoite stage to the host during a blood meal. Within 30–60 minutes, sporozoites invade liver cells, where they replicate and divide as merozoites. The infected liver cell ruptures, releasing the merozoites into the bloodstream, where they invade red blood cells and begin the asexual reproductive stage, which is the symptomatic stage of the disease. Symptoms develop 4–8 days after the initial red blood cell invasion. The replication cycle of the merozoites within the red blood cells lasts 36–72 hours (from red blood cell invasion to haemolysis). Thus, in synchronous infections (infections that originate from a single infectious bite), fever occurs every 36–72 hours, when the infected red blood cells lyse and release endotoxins en masse70–72. Plasmodium vivax and Plasmodium ovale can also enter a dormant state in the liver, the hypnozoite. Merozoites released from red blood cells can invade other red blood cells and continue to replicate, or in some cases, they differentiate into male or female gametocytes4,5. The transcription factor AP2-G (not shown) has been shown to regulate the commitment to gametocytogenesis. Gametocytes concentrate in skin capillaries and are then taken up by the mosquito vector in another blood meal. In the gut of the mosquito, each male gametocyte produces eight microgametes after three rounds of mitosis; the female gametocyte matures into a macrogamete. Male microgametes are motile forms with flagellae and seek the female macrogamete. The male and female gametocytes fuse, forming a diploid zygote, which elongates into an ookinete; this motile form exits from the lumen of the gut across the epithelium254 as an oocyst. Oocysts undergo cycles of replication and form sporozoites, which move from the abdomen of the mosquito to the salivary glands. Thus, 7–10 days after the mosquito feeds on blood containing gametocytes, it may be ‘armed’ and able to infect another human with Plasmodium spp. with her bite. Drugs that prevent Plasmodium spp. invasion or proliferation in the liver have prophylactic activity, drugs that block the red blood cell stage are required for the treatment of the symptomatic phase of the disease, and compounds that inhibit the formation of gametocytes or their development in the mosquito (including drugs that kill mosquitoes feeding on blood) are transmission-blocking agents. *Merozoite invasion of red blood cells can be delayed by months or years in case of hypnozoites. ‡The number of days until symptoms are evident. §The duration of gametogenesis differs by species. ||The maturation of sporozoites in the gut of the mosquito is highly temperature-dependent. Adapted with permission from Ref. 255, Macmillan Publishers Ltd.
The consequences of Plasmodium spp. infection vary in severity depending on the species and on host factors, including the level of host immunity, which is linked to the past extent of parasite exposure7,8. Malaria is usually classified as asymptomatic, uncomplicated or severe (complicated)9 (Box 1). Typical initial symptoms are low-grade fever, shaking chills, muscle aches and, in children, digestive symptoms. These symptoms can present suddenly (paroxysms), and then progress to drenching sweats, high fever and exhaustion. Malaria paroxysmal symptoms manifest after the haemolysis of Plasmodium spp.-invaded red blood cells. Severe malaria is often fatal, and presents with severe anaemia and various manifestations of multi-organ damage, which can include cerebral malaria8 (Box 1). Severe malaria complications are due to microvascular obstruction caused by the presence of red blood cell-stage parasites in capillaries8,10,11. This Primer focuses on our understanding of malaria pathology in the context of parasite and vector biology, progress in diagnostics and new treatments (drugs and vaccines), chemoprotection and chemoprevention.
Epidemiology
The vector
Human malaria parasites are transmitted exclusively by ∼40 species of the mosquito genus Anopheles12. During Anopheles spp. mating, males transfer high levels of the steroid hormone 20-hydroxyecdysone to the females, and the presence of this hormone has been associated with favourable conditions for Plasmodium spp. development13. Malaria-competent Anopheles spp. are abundant and distributed all over the globe, including the Arctic. However, the efficacy of malaria transmission depends on the vector species and, therefore, varies considerably worldwide; for example, in tropical Africa, Anopheles gambiae is a major and highly efficient vector14. The first WHO Global Malaria Eradication Programme (1955–1972) involved, in addition to chloroquine-based treatments, large-scale insecticide campaigns using dichlorodiphenyltrichloroethane (DDT)15. This strategy was quite effective against P. falciparum; although the mosquitoes gradually repopulated DDT-treated areas (because they developed resistance to the insecticide, and the use of DDT itself waned owing to its costs and increasing environmental concerns), these areas have often remained malaria-free and in some cases still are. More-selective vector control approaches, such as the use of insecticide-treated bed nets and indoor residual spraying, have eliminated malaria from several areas (see Diagnosis, screening and prevention, below). However, mosquito resistance to insecticides is a growing concern. Of the 78 countries that monitor mosquito resistance to insecticides, 60 have reported resistance to one or more insecticides since 2010 (Ref. 16).
The parasite
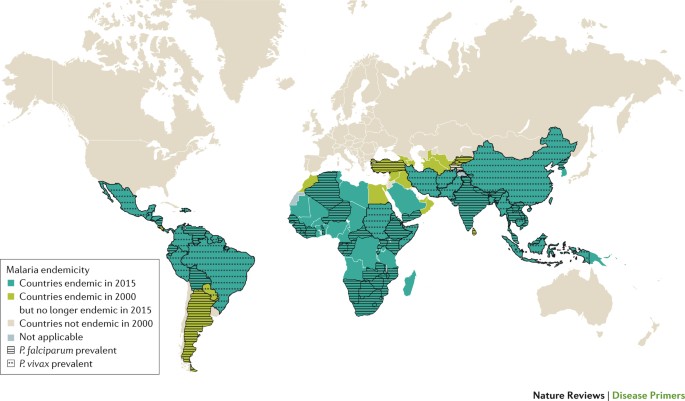
Plasmodium spp. are single-celled eukaryotic organisms17–19 that belong to the phylum Apicomplexa, which is named for the apical complex that is involved in host cell invasion. A discussion of the parasite genome and the genetic approaches used to study parasite biology is provided in Box 2. Of the five human-infective Plasmodium spp., P. falciparum causes the bulk of malaria-associated morbidity and mortality in sub-Saharan Africa, with mortality peaking in the late 1990s at over 1 million deaths annually in the continent20 (Fig. 2). P. falciparum is associated with severe malaria and complications in pregnancy (Box 3); most malaria-related deaths are associated with this species, which kills ∼1,200 African children <5 years of age each day21. However, P. falciparum is also found in malarious tropical areas around the world. P. vivax is found in malarious tropical and temperate areas, primarily Southeast Asia, Ethopia and South America, and generally accounts for the majority of malaria cases in Central and South America and in temperate climates. This distribution can be explained by the fact that P. vivax can survive in climatically unfavourable regions and can stay dormant in a hypnozoite form in its human host's liver for many years. Furthermore, many Africans are negative for the Duffy antigen (also known as atypical chemokine receptor 1) on the surface of red blood cells, and this genotype provides protection from P. vivax malaria, as it makes it more difficult for P. vivax to bind to and penetrate red blood cells22. However, some cases of P. vivax transmission to Duffy antigen-negative individuals have been reported, which suggests that alternative mechanisms of invasion might be present in some strains, and this might portend the escalation of P. vivax malaria to Africa23,24. P. ovale is also found in Africa and Asia, but is especially prevalent in West Africa. Two sympatric species exist: P.o. curtisi and P.o. wallikeri25. Plasmodium malariae — which can be found worldwide but is especially prevalent in West Africa — causes the mildest infections, although it has been associated with splenomegaly or renal damage upon chronic infection. Plasmodium knowlesi — which was initially considered as a parasite of non-human primates — can not only cause malaria in humans but can also lead to severe and even fatal malaria complications26,27. The reasons for the emergence of P. knowlesi in humans are not yet fully understood but are possibly linked to land-use changes that have brought humans into close contact with P. knowlesi-infected mosquitoes28. Regardless, the possible recent emergence of a form of malaria as a zoonosis poses obvious complications for elimination. In addition, co-infections between P. falciparum and P. vivax have been well-documented and have been reported to occur in up to 10–30% of patients living in areas where both parasites are prevalent29,30. Mixed infections can also include other species such as P. ovale and P. malariae, and newer diagnostic methods are being developed that will enable better assessment of the frequency and distribution of these types of co-infection (for example, Ref. 31).
The most-deadly malaria parasite, Plasmodium falciparum, is only found in tropical areas because its gametocytes require 10–18 days at a temperature of >21°C to mate and mature into infectious sporozoites inside the vector256. This development timeline is only possible in hot, tropical conditions; where the ambient temperature is lower, mosquitoes can still propagate, but sporozoite maturation is slowed down and, therefore, incomplete, and parasites perish without progeny when the mosquitoes die. Thus, P. falciparum is quite temperature-sensitive; a global temperature rise of 2–3 °C might result in an additional 5% of the world population (that is, several hundred million people) being exposed to malaria257. Of note, Plasmodium vivax and Plasmodium ovale can develop in mosquitoes at ambient temperatures as low as 16 °C. The abilities of these parasites to propagate at subtropical temperatures and to remain in the hypnozoite state in the liver are likely to explain their ability to survive dry or cold seasons, and the broader global distribution of these parasites258. Countries coded ‘not applicable’ in the Figure were not separately surveyed. Figure based on data from Ref. 16, WHO.
The disease
Malaria remains a major burden to people residing in resource-limited areas in Africa, Asia and Central and South America (Fig. 2). An estimated 214 million cases of malaria occurred in 2015 (Ref. 16). Africa bears the brunt of the burden, with 88% of the cases, followed by Southeast Asia (10%), the eastern Mediterranean region (2%) and Central and South America (<1%). Malaria continues to kill over three-times as many people as all armed conflicts; in 2015, there were an estimated 438,000 (Ref. 16) — 631,000 (Ref. 20) deaths resulting from malaria, compared with an estimated 167,000 deaths due to armed conflicts32,33. In areas of continuous transmission of malaria, children <5 years of age and the fetuses of infected pregnant women experience the most morbidity and mortality from the disease. Children >6 months of age are particularly susceptible because they have lost their maternal antibodies but have not yet developed protective immunity. In fact, adults and children >5 years of age who live in regions of year-round P. falciparum transmission develop a partial protective immunity owing to repeated exposure to the parasite. There is evidence that immunity against P. vivax is acquired more quickly34. Individuals with low protective immunity against P. falciparum are particularly vulnerable to severe malaria. Severe malaria occurs in only 1% of infections in African children and is more common in patients who lack strong immune protection (for example, individuals who live in low-transmission settings, children <5 years of age and naive hosts). Severe malaria is deadly in 10% of children and 20% of adults7. Pregnant women are more susceptible to Plasmodium spp. infection because the placenta itself selects for the emergence of parasites that express receptors that recognize the placental vasculature; these receptors are antigens to which pregnant women have not yet become partially immune7 (Box 3). This vulnerability increases the risk of miscarriage; parasitaemia in the placenta can have adverse effects on the fetus35–37 (Box 3).
Co-infection of Plasmodium spp. with other pathogens — including HIV, Mycobacterium tuberculosis and helminths — is common. HIV-infected adults are at an increased risk of severe malaria and death38. The overall prevalence of helminth infection is very high (>50% of the population) in malaria-endemic regions and is associated with increased malaria parasitaemia39. Surprisingly, naturally occurring iron deficiency and anaemia protect against severe malaria, which was an unexpected finding40, as numerous clinical studies have aimed to fortify children and prevent anaemia by distributing iron supplements41.
From 2000 to 2015, the incidence of malaria fell by 37% and the malaria mortality rate fell by 60% globally16. The WHO attributes much of this reduction of malaria-associated morbidity and mortality to the scale-up of three interventions: insecticide-treated bed nets (69% of the reduction), artemisinin-based combination therapies (ACTs; 21%) and indoor residual insecticide spraying (10%)16 (see Diagnosis, screening and prevention, below). Until ACT was introduced, progress in malaria control in most malarious countries was threatened or reversed by the nearly worldwide emergence of chloroquine-resistant and sulfadoxine–pyrimethamine-resistant P. falciparum strains and, more recently, of other resistant Plasmodium spp. ACT has become the antimalarial medicine of choice in most malarious areas, and demonstrates rapid parasite clearance, superior efficacy (compared with other clinically approved drugs) and >98% cure rates (typically defined as the percentage of patients who remain malaria-free for 28 days; re-infection events do not count as a recurrence). ACTs achieve these results even in strains that are resistant to older antimalarials, effectively turning the tide against antimalarial drug resistance. However, the emergence of artemisinin-resistant strains in Southeast Asia threatens the usefulness of ACTs42–45 (see Drug resistance, below).
Mechanisms/pathophysiology
The red blood cell stage
As previously mentioned, the red blood cell stage of Plasmodium spp. infection is the cause of symptomatic malaria, as red blood cells are the site of abundant parasite replication.
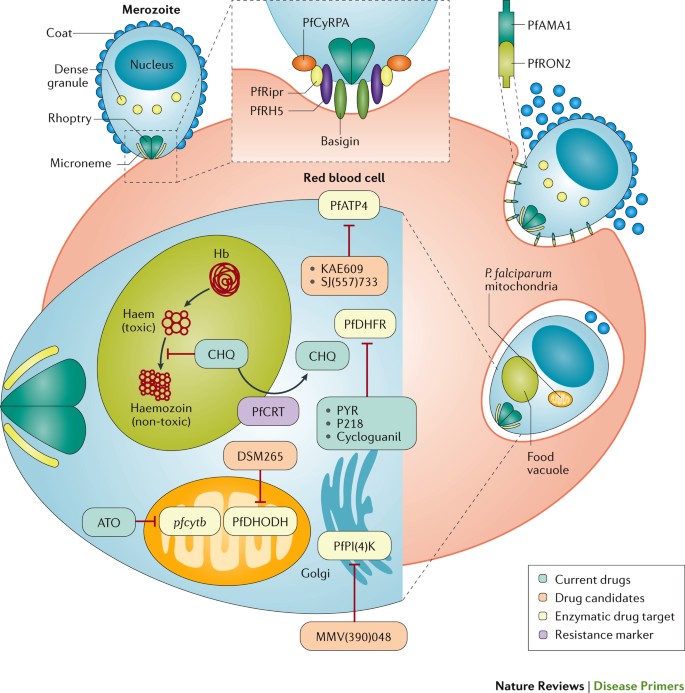
Invasion. Plasmodium spp. parasites gain entry into the red blood cell through specific ligand–receptor interactions mediated by proteins on the surface of the parasite that interact with receptors on the host erythrocyte (mature red blood cell) or reticulocyte (immature red blood cell)46 (Fig. 3). Whereas P. falciparum can invade and replicate in erythrocytes and reticulocytes, P. vivax and other species predominantly invade reticulocytes, which are less abundant than erythrocytes47. Most of the parasite erythrocyte-binding proteins or reticulocyte-binding proteins that have been associated with invasion are redundant or are expressed as a family of variant forms; however, for P. falciparum, two essential red blood cell receptors (basigin and complement decay-accelerating factor (also known as CD55)) have been identified (Fig. 3).
Invasion occurs through a multistep process259. During pre-invasion, low-affinity contacts are formed with the red blood cell membrane. Reorientation of the merozoite is necessary to enable close contact between parasite ligands and host cell receptors, and this is then followed by tight junction formation. In Plasmodium falciparum, a forward genetic screen has shown that complement decay-accelerating factor (not shown) on the host red blood cell is essential for the invasion of all P. falciparum strains260. The interaction of a complex of P. falciparum proteins (reticulocyte-binding protein homologue 5 (PfRH5), PfRH5-interacting protein (PfRipr) and cysteine-rich protective antigen (PfCyRPA)) with basigin on the red blood cell surface is also essential for the invasion in all strains261,262. PfRH5 has been studied as a potential vaccine candidate46, and antibodies against basigin have been considered as a potential therapeutic strategy263. During the PfRH5–PfRipr–PfCyRPA–basigin binding step, an opening forms between the parasite and the red blood cell, and this triggers Ca2+ release and enables parasite-released proteins to be inserted into the red blood cell membrane. These proteins are secreted from the micronemes (the small secretory organelles that cluster at the apical end of the merozoite) and from the neck of the rhoptries, and include rhoptry neck protein 2 (PfRON2). Binding between PfRON2 and apical membrane antigen 1 (PfAMA1) on the merozoite surface is required to mediate tight junction formation before the internalization process264, and PfAMA1 is also being evaluated as a vaccine candidate265. Parasite replication within the red blood cell requires the synthesis of DNA, which can be blocked by several antimalarials: pyrimethamine (PYR), P218 and cycloguanil target P. falciparum dihydrofolate reductase (PfDHFR)266, and atovaquone (ATO) blocks pyrimidine biosynthesis by inhibiting the expression of the mitochondrial gene pfcytb (which encodes P. falciparum cytochrome b) and by preventing the formation of oxidized coenzyme Q, which is needed to enable the pyrimidine biosynthetic enzyme dihydroorotate dehydrogenase (PfDHODH) to perform its reaction within the mitochondria50. The phase II clinical candidate DSM265 also blocks pyrimidine biosynthesis by directly inhibiting PfDHODH186. In addition to DNA synthesis, other processes can be targeted by antimalarial drugs. Chloroquine (CHQ) inhibits haem polymerization in the food vacuole52 but can be expelled from this compartment by the P. falciparum chloroquine-resistance transporter (PfCRT)267. The phase II clinical candidate KAE609 and the preclinical candidate SJ(557)733 both inhibit P. falciparum p-type ATPase 4 (PfATP4), which is required for Na+ homeostasis during nutrient acquisition57,183,184. The phase I clinical candidate MMV(390)048 (Ref. 191) inhibits P. falciparum phosphatidylinositol 4-kinase (PfPI(4)K), which is required for the generation of transport vesicles that are needed to promote membrane alterations during ingression58. Hb, haemoglobin.
Replication. Once Plasmodium spp. gain entry into the red blood cell, they export hundreds of proteins into the host cell cytoplasm and cell surface that modulate the acquisition of nutrients, cell adhesion and sequestration in tissues, and pathogenesis3,48,49. Molecular and cell biology approaches are expanding our understanding of the molecular machinery that is required for the export, as well as the identification and function of the exported proteins.
In the red blood cell, Plasmodium spp. replicate rapidly, and during symptomatic disease the parasites may replicate exponentially to >1012 parasites per patient. This rapid growth requires sustained pools of nucleotides for the synthesis of DNA and RNA, and as a consequence, many antimalarials target pyrimidine biosynthesis50 (Fig. 3). Plasmodium spp. are auxotrophic for all of the amino acids they need (that is, they must acquire all of these from food because they cannot synthesize them from precursors). Haemoglobin digestion (in a specialized food vacuole) supplies all amino acids except isoleucine, which must be obtained from other host cell components51. Haemoglobin digestion also releases haem, which is toxic to the parasite and, therefore, is polymerized into haemozoin (often called malaria pigment, which is visible as a blue pigment under light microscopy), which is an insoluble crystal that sequesters the toxic metabolite52. How haem polymerization is facilitated by the parasite remains unclear. A complex of several proteases and haem detoxification protein (HDP) have been identified in the food vacuole; follow-up in vitro studies have shown that components of this complex (for example, falcipain 2, HDP and lipids) were able to catalyse the conversion of haem into haemozoin53. The importance of understanding this mechanism is highlighted by the finding that chloroquine and other antimalarials act by inhibiting haem polymerization54 (Fig. 3). There is also evidence that the iron (haem-bound or free) liberated in the food vacuole during haemoglobin digestion plays a part in activating the toxicity to the parasite of artemisinin derivatives42.
Nutrient uptake by the parasite is coupled to the detrimental accumulation of Na+; however, the parasite expresses an essential plasma membrane Na+ export pump (the cation ATPase P. falciparum p-type ATPase 4 (PfATP4)) that can maintain Na+ homeostasis55–57 (Fig. 3). The remodelling of the plasma membrane (membrane ingression) to generate daughter merozoites in the late schizont stage requires P. falciparum phosphatidylinositol 4-kinase (PfPI(4)K)58. Both PfPI(4)K and PfATP4 are targets of new drugs that are under development (Fig. 3).
Immune evasion and host immunity
Malaria parasites first encounter the host immune system when sporozoites are injected in the skin (measured to be ∼15 per mosquito bite in one study59), where they may be phagocytosed by dendritic cells for antigen presentation in the lymph node draining the skin inoculation site60. The chances of transmission are increased when the host is bitten by mosquitoes that carry a larger number of sporozoites, despite the fact that the number of sporozoites that can simultaneously pass through the mosquito's proximal duct is limited by the duct diameter61. Sporozoites encounter several other effectors of the immune system, and how a minority of them can reach the liver and infect the hepatocytes is not well understood. Immune evasion in the liver could be in part explained by the ability of sporozoites to suppress the function of Kupffer cells (also known as stellate macrophages, which are the resident macrophages of the liver) and repress the expression of genes that encode MHC class I molecules62. Our understanding of the host immunity associated with the red blood cell stage is more complete. Virulence genes in Plasmodium spp. are part of large expanded multigene families that are found in specialized (for example, subtelomeric) regions of the chromosomes7,63,64. These gene families (for example, var genes in P. falciparum) encode variants of cell surface proteins that function in immune evasion through antigenic variation and also are involved in mediating cytoadherence of infected red blood cells to endothelial cells, which leads to red blood cell sequestration in tissues.
Malaria disease severity — in terms of both parasite burden and the risk of complicated malaria — is dependent on the levels of protective immunity acquired by the human host65–67, which can help to decrease the severity of symptoms and reduce the risk of severe malaria. Immunity is thought to result from circulating IgG antibodies against surface proteins on sporozoites (thereby blocking hepatocyte invasion) and merozoites (thereby blocking red blood cell invasion). In high-transmission areas where malaria is prevalent year-round, adults develop partially protective immunity. Young infants (<6 months of age) are also afforded some protection, probably from the antibodies acquired from their mother, whereas children from 6 months to 5 years of age have the lowest levels of protective immunity and are the most susceptible to developing high parasitaemia with risks for complications and death (for example, see the study conducted in Kilifi, Kenya68). In low-transmission areas or areas that have seasonal malaria, individuals develop lower levels of protective immunity and typically have worse symptomatic malaria upon infection. This correlation between protective immunity and malaria severity poses a challenge for successful malaria treatment programmes; as the number of infections and the transmission rates decrease, increasing numbers of patients will lose protective immunity and become susceptible to severe disease. The re-introduction of malaria in areas that had been malaria-free for many years could be devastating in the short term and, therefore, well-organized surveillance is required.
Pathogenesis
The predominant pathogenic mechanism is the haemolysis of Plasmodium spp.-infected red blood cells, which release parasites and malaria endotoxin — understood to be a complex of haemozoin and parasite DNA, which trigger Toll-like receptor 9 (TLR9), a nucleotide-sensing receptor involved in the host immune response against pathogens69 — that leads to high levels of tumour necrosis factor (TNF) production and to clinical symptoms such as fever70–72. In addition, the membrane of infected red blood cells stiffens, and this loss of deformability contributes to the obstruction of capillaries, which has life-threatening consequences in severe malaria when vital organs are affected73.
Parasite factors that influence disease severity. Disease severity and pathogenesis are linked to surface proteins that are expressed by the parasite. In P. falciparum, a major surface antigen is encoded by the var gene family, which contains ∼60 members7,11,63,64. The majority of the var genes are classified into three subfamilies — A, B and C — on the basis of their genomic location and sequence: the B and C groups mediate binding to host cells via CD36 (also known as platelet glycoprotein 4), whereas the A group genes mediate non-CD36 binding interactions that have been linked to severe malaria, including cerebral malaria7,64. The var genes encode P. falciparum erythrocyte membrane protein 1 (PfEMP1), with the B and C groups accounting for >80% of PfEMP1 variants. PfEMP1 is the major protein involved in cytoadherence and mediates the binding of infected erythrocytes to the endothelial vasculature. In cerebral malaria, A group PfEMP1 variants mediate the binding of infected erythrocytes to endothelial protein C receptor (EPCR) and intercellular adhesion molecule 1 (ICAM1) in the brain, causing pathology8,11,74,75. However, our knowledge of the host cell receptors that are involved in interactions with the infected erythrocytes is probably incomplete. For example, thrombin — which regulates blood coagulation via vitamin K-dependent protein C — can cleave PfEMP1, thereby reversing and preventing the endothelial binding of infected erythrocytes74. In pregnancy, the expression of a specific PfEMP1 variant, variant surface antigen 2-CSA (VAR2CSA) — which is not encoded by one of the three main subfamilies — leads to an increased risk of placental malaria7,64 (Box 3).
High parasitaemia levels also seem to correlate with poor outcomes7,75, and the circulating levels of P. falciparum histidine-rich protein 2 (which is encoded by pfhrp2) have been used as a biomarker of parasitaemia that predicts the risks for microvascular obstruction and severe disease76. The brain pathology in children with severe malaria has recently been described in detail77.
Additionally, P. vivax does not express the same family of var genes that have been found to be strongly associated with endothelium binding and tissue sequestration, which drives severe disease in P. falciparum, and the ability of P. vivax to only invade reticulocytes leads to lower parasite levels7.
Host traits that influence disease severity. Malaria has exerted a strong selection pressure on the evolution of the human genome78,79. Some haemoglobin-encoding alleles that in homozygous genotypes cause severe blood disorders (such as thalassaemia, the earliest described example, and sickle cell disease) have been positively selected in populations living in malaria-endemic areas because heterozygous genotypes protect against malaria80. Other inherited haemoglobin abnormalities (for example, mutations affecting haemoglobin C and haemoglobin E) can also provide protection against malaria81.
In addition, genetic polymorphisms that affect proteins expressed by red blood cells or that lead to enzyme deficiencies can also be protective against severe disease. The red blood cell Duffy antigen is a key receptor that mediates the invasion of P. vivax through interaction with the Duffy antigen-binding protein on the parasite surface46. The genetic inheritance of mutations in ACKR1 (which encodes the Duffy antigen) in Africa is credited with reducing the spread of P. vivax in this continent, although the finding of Duffy antigen-negative individuals who can be infected with P. vivax suggests that we still have an incomplete understanding of the factors involved in P. vivax invasion82,83. Glucose-6-phosphate dehydrogenase (G6PD) deficiency78,79 provides protection against severe malaria through an unknown mechanism, at least in hemizygous males84, but unfortunately also leads to haemolytic anaemia in patients treated with primaquine, which is an 8-aminoquinoline antimalarial and the only agent currently approved for the treatment of latent (liver-stage) P. vivax malaria. The mode of action of primaquine, which is a prodrug, remains unknown.
The mechanisms of malaria protection in these varied genetic disorders have been widely studied81. Common findings include increased phagocytosis and elimination by the spleen of infected mutant erythrocytes, which reduces parasitaemia; reduced parasite invasion of mutant red blood cells; reduced intracellular growth rates; and reduced cytoadherence of infected mutant red blood cells. All of these effects increase protection against severe malaria, which is the main driver of human evolution in this case. Some point mutations in the gene that encodes haemoglobin alter the display of PfEMP1 on the surface of infected red blood cells, thereby diminishing cytoadherence to endothelial cells85,86. This finding highlights the crucial role of cytoadherence in promoting severe disease.
Finally, variability in the response to TNF, which is secreted from almost all tissues in response to malaria endotoxins, has also been proposed as a factor that mediates differential host responses and contributes to severe malaria when levels are high7.
Diagnosis, screening and prevention
Diagnosis
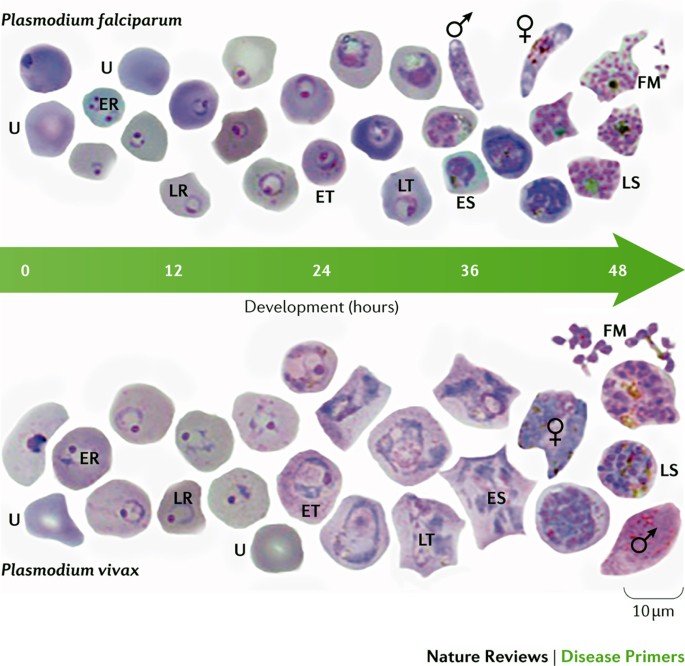
The WHO criteria for the diagnosis of malaria consider two key aspects of the disease pathology: fever and the presence of parasites87. Parasites can be detected upon light microscopic examination of a blood smear (Fig. 4) or by a rapid diagnostic test (RDT)87. The patient's risk of exposure (for example, whether the patient lives in an endemic region or their travel history) can assist in making the diagnosis. Furthermore, the clinical expression of Plasmodium spp. infection correlates with the species’ level of transmission in the area. The symptoms of uncomplicated malaria include sustained episodes of high fever (Box 1); when high levels of parasitaemia are reached, several life-threatening complications might occur (severe malaria) (Box 1).
Thin blood films showing Plasmodium falciparum (upper panel) and Plasmodium vivax (lower panel) at different stages of blood-stage development. The images are from methanol-fixed thin films that were stained for 30 minutes in 5% Giemsa. The samples were taken from Thai and Korean patients with malaria: Ethical Review Committee for Research in Human Subjects, Ministry of Public Health, Thailand (reference no. 4/2549, 6 February 2006). The sex symbols represent microgametes (male symbol) and macrogametes (female symbol). ER, early ring stage; ES, early schizont stage; ET, early trophozoite stage; FM, free merozoites; LR, late ring stage; LS, late schizont stage; LT, late trophozoite stage; U, uninfected red blood cell. The slides used were from a previously published study268 but the images shown have not been previously published. Images courtesy of A.-R. Eruera and B. Russell, University of Otago, New Zealand.
The complications of severe malaria mostly relate to the blocking of blood vessels by infected red blood cells, with the severity and symptoms depending on what organ is affected (Box 1) and to what extent, and differ by age; lung and kidney disease are unusual in children in Africa but are common in non-immune adults.
Parasitaemia. Patients with uncomplicated malaria typically have parasitaemia in the range of 1,000–50,000 parasites per microlitre of blood (however, non-immune travellers and young children who have parasite numbers <1,000 can also present with symptoms). The higher numbers tend to be associated with severe malaria, but the correlation is imprecise and there is no cut-off density. In a pooled analysis of patient data from 61 studies that were designed to measure the efficacy of ACTs (throughout 1998–2012), parasitaemia averaged ∼4,000 parasites per microlitre in South America, ∼10,000 parasites per microlitre in Asia and ∼20,000 parasites per microlitre in Africa88. The limit of detection by thick-smear microscopy is ∼50 parasites per microlitre89. WHO-validated RDTs can detect 50–1,000 parasites per microlitre with high specificity, but many lack sensitivity, especially when compared with PCR-based methods90. The ability to detect low levels of parasitaemia is important for predicting clinical relapses, as parasitaemia can increase 20-fold over a 48-hour cycle period. These data are based on measurements in healthy volunteers (controlled human infection models) who were infected at a defined time point with a known number or parasites, and in whom the asymptomatic parasite reproduction was monitored by quantitative PCR up to the point at which the individual received rescue treatment91.
In hyperendemic areas (with year-round disease transmission), often many children and adults are asymptomatic carriers of the parasite. In these individuals, the immune system maintains parasites at equilibrium levels in a ‘tug-of-war’. However, parasitaemia in asymptomatic carriers can be extremely high, with reports of levels as high as 50,000 parasites per microlitre in a study of asymptomatic pregnant women (range: 80–55,400 parasites per microlitre)92. In addition to the obvious risks for such people, they represent a reservoir for infecting mosquitoes, leading to continued transmission. In clinical studies, the parasitaemia of asymptomatic carriers can be monitored using PCR-based methods, which can detect as few as 22 parasites per millilitre93. However, the detection of low-level parasitaemia in low-resource settings requires advanced technology. Loop-mediated isothermal amplification (LAMP)94 is one promising approach. This type of PCR is fast (109-fold amplification in 1 hour) and does not require thermal cycling, which reduces the requirement for expensive hardware. Versions of this method that do not require electricity are being developed95. Nucleic acid-based techniques such as LAMP and PCR-based methods also have the advantage that they can be used to detect multiple pathogens simultaneously and, in theory, identify drug-resistant strains96. This approach enables the accurate diagnosis of which Plasmodium spp. is involved, and in the future could lead to the development of multiplexed diagnostics that enable differential diagnosis of the causative pathogens (including bacteria and viruses) in patients who present with fever97.
RDTs. RDTs are based on the immunological detection of parasite antigens (such as lactate dehydrogenase (LDH) or histidine-rich protein 2) in the blood, have sensitivities comparable to that of light microscopy examination and have the advantage that they do not require extensive training of the user. These tests provide rapid diagnosis at a point-of-care level in resource-limited settings and can, therefore, substantially improve malaria control. However, occasionally, false-positive results from RDTs can be problematic because they could lead to the wrong perception that antimalarial medicines are ineffective. False-negative test results have been reportedly caused by pfhrp2 gene deletions in P. falciparum strains in South America98–103. Current data indicate that LDH-targeting RDTs are less sensitive for P. vivax than for P. falciparum104, and limited information on the sensitivity of these tests for the rarer species, such as P. ovale or P. malariae, is available. RDTs also offer a great opportunity to track malaria epidemiology; photos taken with mobile phones of the results of the tests can be uploaded to databases (even using cloud-based data architecture105) and provide an automated collection of surveillance data106.
Prevention in vulnerable populations
The prevention of Plasmodium spp. infection can be accomplished by different means: vector control, chemoprevention and vaccines. Mosquito (vector) control methods include the following (from the broadest to the most targeted): the widespread use of insecticides, such as DDT campaigns; the use of larvicides; the destruction of breeding grounds (that is, draining marshes and other breeding reservoirs); indoor residual spraying with insecticides (that is, the application of residual insecticide inside dwellings, on walls, curtains or other surfaces); and the use of insecticide-treated bed nets. The use of endectocides has also been proposed; these drugs, such as ivermectin, kill or reduce the lifespan of mosquitoes that feed on individuals who have taken them107. However, this approach is still experimental; individuals would be taking drugs that have no direct benefit to themselves (as they do not directly prevent human illness), and so the level of safety data required for the registration of endectocides for this purpose will need to be substantial. Vector control approaches differ in terms of their efficacy, costs and the extent of their effect on the environment. Targeted approaches such as insecticide-treated bed nets have had a strong effect. Chemoprevention is an effective strategy that has been used to reduce malaria incidence in campaigns of seasonal malaria chemoprevention, in intermittent preventive treatment for children and pregnant women, and for mass drug administration108. Such antimalarials need to have an excellent safety profile as they are given to large numbers of healthy people. Vaccines excel in eradicating disease, but effective malaria vaccines are challenging because — unlike viruses and bacteria, against which effective vaccines have been developed — protist pathogens (such as Plasmodium spp.) are large-genome microorganisms that have evolved highly effective immune evasion strategies (such as encoding dozens or hundreds of cell surface protein variants). Nevertheless, the improved biotechnological arsenal to generate antigens and improved adjuvants could help to overcome these issues.
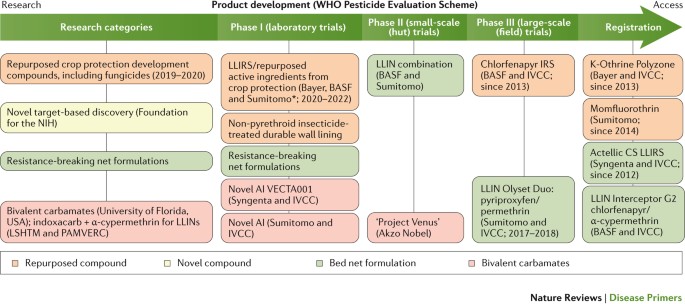
Vector control measures. The eradication of mosquitoes is no longer considered an option to eliminate malaria; however, changing the capacity of the vector reservoir has substantial effects on malaria incidence. Long-lasting insecticide-treated bed nets and indoor residual spraying have been calculated to be responsible for two-thirds of the malaria cases averted in Africa between 2000 and 2015 (Ref. 12). Today's favoured and more-focused vector control approach involves the use of fine-mazed, sturdy, long-lasting and wash-proof insecticide-treated bed nets109. The fabric of these nets is impregnated with an insecticide that maintains its efficacy after ≥20 standardized laboratory washes, and these nets have a 3-year recommended use. Insects are attracted by the person below the net but are killed as they touch the net. However, the efficacy of bed nets is threatened by several factors, including their inappropriate use (for example, for fishing purposes) and behavioural changes in the mosquitoes, which have also begun to bite during the day110. The main problem, however, is the increasing emergence of vector resistance to insecticides, especially pyrethroids110 and, therefore, new insecticides with different modes of action are urgently needed. New insecticides have been identified by screening millions of compounds from the libraries of agrochemical companies, but even those at the most advanced stages of development are still 5–7 years from deployment (see the International Vector Control Consortium website (http://www.ivcc.com) and Ref. 111) (Fig. 5). Few of these new insecticides are suitable for application in bed nets (because of high costs or unfavourable chemical properties), but some can be used for indoor residual spraying. New ways of deploying these molecules are also being developed, such as improved spraying technologies112, timed release to coincide with seasonal transmission and slow-release polymer-based wall linings113,114.
The categories of compounds that are currently under study are defined in the first column on the left; compounds belonging to these categories have advanced to phase I trials or later stages. New screening hits (developed by Syngenta, Bayer, Sumitomo and the Innovative Vector Control Consortium (IVCC)) are at early research stages and are not expected to be deployed until 2020–2022. Similarly, species-specific approaches to the biological control of mosquitoes are not expected to move forward before 2025. The main data source for this Figure was the IVCC; for the latest updates visit the IVCC website (www.ivcc.com). Note that not all compounds listed on the IVCC website are shown in this Figure. The dates reflect the expected deployment dates. AI, active ingredient; CS, capsule suspension; IRS, indoor residual spray; LLIN, long-lasting insecticidal mosquito net; LLIRS, long-lasting indoor residual spray; LSHTM, London School of Hygiene and Tropical Medicine (UK); PAMVERC, Pan-African Malaria Vector Research Consortium. *Clothianidin and chlorfenapyr.
Genetic approaches, fuelled by advances in the CRISPR–Cas9 gene editing technology, represent an exciting area of development for novel insect control strategies. There are currently two main approaches: population suppression, whereby mosquitoes are modified so that any progeny are sterile; and population alteration, whereby mosquitoes are modified so that the progeny are refractory to Plasmodium spp. infection115,116. Initial approaches to population suppression involved releasing sterile male insects117. These strategies have now been developed further, with the release of male insects carrying a dominant lethal gene that kills their progeny118,119. Gene drive systems can be used for both population suppression and population alteration. These systems use homing endonucleases, which are microbial enzymes that induce the lateral transfer of an intervening DNA sequence and can, therefore, convert a heterozygote individual into a homozygote. Homing endonucleases have been re-engineered to recognize mosquito genes120 and can rapidly increase the frequency of desirable traits in a mosquito population121. Gene drive systems have now been used in feasibility studies to reduce the size of mosquito populations122 or to make mosquitoes less able to transmit malaria-causing parasites123. Another approach is inspired by the finding that Aedes aegypti mosquitoes (the vector for Dengue, yellow fever and Zika viruses) infected with bacteria of the Wolbachia spp. (a parasite that naturally colonizes numerous species of insects) cannot transmit the Dengue virus to human hosts124. Symbiont Wolbachia spp. can be modified to make them deleterious to other parasites in the same host, and progress has been made in finding symbionts that can colonize Anopheles spp. mosquitoes125,126. Although all of the above approaches are very promising, they are still at a very early stage, and the environmental uncertainties associated with the widespread distribution of such technologies, as well as the complex regulatory requirements, provide additional hurdles that will need to be overcome.
Chemoprotection and chemoprevention. Chemoprotection describes the use of medicines (given at prophylactic doses) to temporarily protect subjects entering an area of high endemicity — historically, tourists and military personnel — and populations at risk from emergent epidemics, but is also being increasingly considered for individuals visiting areas that have recently become malaria-free. Chemoprevention, which is often used in the context of seasonal malaria, describes the use of medicines with demonstrated efficacy that are given regularly to large populations at full treatment doses (as some of the individuals treated will be asymptomatic carriers).
Currently, there are three ‘gold-standard’ alternatives for chemoprotection: daily atovaquone–proguanil, daily doxycycline and weekly mefloquine. Mefloquine is the current mainstay drug used to prevent the spread of multidrug-resistant Plasmodium spp. in the Greater Mekong subregion of Southeast Asia, despite having a ‘black box warning’ for psychiatric adverse events; however, an analysis of pooled data from 20,000 well-studied patients found that this risk was small (<12 cases per 10,000 treatments)127. An active search to find new medicines that could be useful in chemoprotection, in particular medicines that can be given weekly or even less frequently, is underway. One interesting possibility is the use of long-acting injectable intramuscular combination chemoprotectants, which, if effective, could easily compete with vaccination, if they provided protection with 3–4 injections per year. Such an approach (called pre-exposure prophylaxis) is being studied for HIV infection (which also poses major challenges to the development of an effective vaccine)128 and may lead to the development of long-acting injectable drug formulations129 produced as crystalline nanoparticles (to enhance water solubility) using the milling technique.
Chemoprevention generally refers to seasonal malaria chemoprevention campaigns, which target children <5 years of age130. In the Sahel region (the area just south of the Sahara Desert, where there are seasonal rains and a recurrent threat of malaria), seasonal malaria chemoprevention with a combination of sulfadoxine–pyrimethamine plus amodiaquine had a strong effect131–135, with a >80% reduction in the number of malaria cases among children and a >50% reduction in mortality136. Although these campaigns are operationally complex — as the treatment has to be given monthly — >20 million children have been protected between 2015 and 2016, at a cost of ∼US$1 per treatment. A concern about seasonal malaria chemoprevention is the potential for a rebound effect of the disease. Rebound could occur if children lose immunity to malaria while receiving treatment that is later stopped because they reached the age limit, if campaigns are interrupted because of economic difficulties or social unrest (war), or if drug resistance develops. Owing to the presence of resistant strains, a different approach is needed in African areas south of the Equator137, and this led to trials of monthly 3-day courses of ACTs in seasonal chemoprevention135; there is an increasing amount of literature on the impressive efficacy of dihydroartemisinin (DHA)–piperaquine to prevent malaria in high-risk groups138. To reduce the potential for the emergence of drug resistance, the WHO good practice standards state that, when possible, drugs used for chemoprevention should differ from the front-line treatment that is used in the same country or region108, which emphasizes the need for the development of multiple, new and diverse treatments to provide a wider range of options.
Finally, intermittent preventive treatment is also recommended to protect pregnant women in all malaria-endemic areas108 (Box 3).
Vaccines. Malaria, along with tuberculosis and HIV infection, is a disease in which all components of the immune response (both cellular, in particular, during the liver stage, and humoral, during the blood stage) are involved yet provide only partial protection, which means that developing an effective vaccine will be a challenge. The fact that adults living in high-transmission malarious areas acquire partial protective immunity indicates that vaccination is a possibility. As a consequence, parasite proteins targeted by natural immunity, such as the circumsporozoite protein (the most prominent surface antigen expressed by sporozoites), proteins expressed by merozoites and parasite antigens exposed on the surface of infected red blood cells139 have been studied for their potential to be used in vaccine programmes140. However, experimental malaria vaccines tend to target specific parasite species and surface proteins, an approach that both restricts their use and provides scope for the emergence of resistance. Sustained exposure to malaria is needed to maintain natural protective immunity, which is otherwise lost within 3–5 years141, perhaps as a result of the clearance of circulating antibodies and the failure of memory B cells to develop into long-lived plasma B cells. Controlled human infection models142–144 have started to provide a more precise understanding of the early cytokine and T cell responses in naive subjects, emphasizing the role of regulatory T cells in dampening the response against the parasite, which results in the exhaustion of T cells145. Vaccine development is currently focusing on using multiple antigens from different stages of the parasite life cycle. Future work will also need to focus on the nature of the immune response in humans and specifically the factors that lead to diminished T cell responses. New generations of adjuvants are needed, possibly compounds that produce the desired specific response rather than inducing general immune stimulation. This is a challenging area of research, as adjuvants often have a completely different efficacy in humans compared with in preclinical animal models.
Currently, there is no vaccine deployed against malaria. The ideal vaccine should protect against both P. falciparum and P. vivax, with a protective, lasting efficacy of at least 75%. The most advanced candidate is RTS,S (trade name: Mosquirix; developed by GlaxoSmithKline and the Program for Appropriate Technology in Health Malaria Vaccine Initiative), which contains a recombinant protein with parts of the P. falciparum circumsporozoite protein combined with the hepatitis B virus surface antigen and a proprietary adjuvant. RTS,S reduced the number of malaria cases by half in 4,358 children 5–17 months of age during the first year following vaccination146, preventing 1,774 cases for every 1,000 children also owing to herd immunity, and had an efficacy of 40% over the entire 48 months of follow-up in children who received four vaccine doses over a 4-year period147. The efficacy of RTS,S during the entire follow-up period dropped to 26% when children only received three vaccine doses. The efficacy during the first year in 6–12-week-old children was limited to 33%. Thus, the RTS,S vaccine failed to provide long-term protection. Further studies, as requested by the WHO, will be done in pilot implementations of 720,000 children in Ghana, Kenya and Malawi (240,000 in each country, half of whom will receive the vaccine) before a final policy recommendation is made. However, a vaccine with only partial and short-term efficacy could still be used in the fight against malaria. RTS,S could be combined with chemoprevention to interrupt malaria transmission in low-endemic areas148. Thus, vaccines that are unable to prevent Plasmodium spp. infection could be used to prevent transmission (for example, by targeting gametocytes) or used as an additional protective measure in pregnant women.
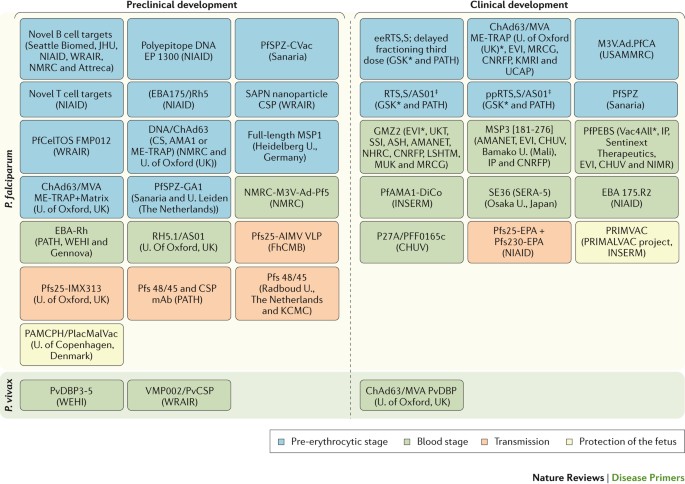
A large pipeline of vaccine candidates is under evaluation (Fig. 6). These include irradiated sporozoites — an approach that maximizes the variety of antigens exposed149 — and subunit vaccines, which could be developed into multicomponent, multistage and multi-antigen formulations150. Although vaccines are typically designed for children, as the malaria map shrinks, both paediatric and adult populations living in newly malaria-free zones will need protection because they would probably lose any naturally acquired immunity and would, therefore, be more susceptible. Indeed, in recent years, there has been a focus on developing transmission-blocking vaccines to drive malaria elimination. This approach has been labelled altruistic, as vaccination would have no direct benefit for the person receiving it, but it would benefit the community; a regulatory pathway for such a novel approach has been proposed151,152. The most clinically advanced vaccine candidate that is based on this approach is a conjugate vaccine that targets the female gametocyte marker Pfs25 (Ref. 153), and other antigens are being tested preclinically. Monoclonal antibodies are another potential tool to provide protection. Improvements in manufacturing and high-expressing cell lines are helping to overcome the major barrier to the use of monoclonal antibodies (high costs)154, and improvements in potency and pharmacokinetics are reducing the volume and frequency of administration155. Monoclonal antibodies could be particularly useful to safely provide the relatively short-term protection needed in pregnancy. The molecular basis of the interaction between parasites and the placenta is quite well understood; two phase I trials of vaccines that are based on the VAR2CSA antigen are under way156,157.
The main data source for this Figure was Ref. 269. Not all vaccines under development are shown in the Figure. AIMV VLP, Alfalfa mosaic virus virus-like particle; AMA1, apical membrane antigen 1; AMANET, African Malaria Network Trust; ASH, Albert Schweitzer Hospital (Gabon); ChAd63, chimpanzee adenovirus 63; CHUV, Centre Hospitalier Universitaire Vaudois (Switzerland); CNRFP, Centre National de Recherche et de Formation sur le Paludisme (Burkina Faso); CS, circumsporozoite protein; CSP, circumsporozoite protein; EBA, erythrocyte-binding antigen; ee, elimination eradication; EP, electroporation; EPA, Pseudomonas aeruginosa exoprotein A; EVI, European Vaccine Initiative; CVac, chemoprophylaxis vaccine; FhCMB, Fraunhofer Center for Molecular Biotechnology (USA); GSK, GlaxoSmithKline; IP, Institut Pasteur (France); INSERM, Institut National de la Santé et de la Recherche Médicale (France); JHU, Johns Hopkins University (USA); KCMC, Kilimanjaro Christian Medical College (Tanzania); KMRI, Kenyan Medical Research Institute; LSHTM, London School of Hygiene and Tropical Medicine (UK); M3V.Ad.PfCA, multi-antigen, multistage, adenovirus-vectored vaccine expressing Plasmodium falciparum CSP and AMA1 antigens; mAb, monoclonal antibody; ME-TRAP multiple epitope thrombospondin-related adhesion protein; MRCG, Medical Research Council (The Gambia); MSP, merozoite surface protein; MVA, modified vaccinia virus Ankara; MUK, Makerere University Kampala (Uganda); NHRC, Navrongo Health Research Centre (Ghana); NIAID, National Institute of Allergy and Infectious Diseases (USA); NIMR, National Institute for Medical Research (UK); NMRC, Naval Medical Research Center (USA); PAMCPH, pregnancy-associated malaria Copenhagen; PATH, Program for Appropriate Technology in Health; PfAMA1-DiCo, diversity-covering Plasmodium falciparum AMA1; PfCelTOS, Plasmodium falciparum cell-traversal protein for ookinetes and sporozoites; PfPEBS, Plasmodium falciparum pre-erythrocytic and blood stage; PfSPZ, Plasmodium falciparum sporozoite; PfSPZ-GA1, genetically attenuated PfSPZ; pp, paediatric prevention; PRIMALVAC, PRIMVAC project (INSERM); PRIMVAC, recombinant var2CSA protein as vaccine candidate for placental malaria; Pfs25, Plasmodium falciparum 25 kDa ookinete surface antigen; PvCSP, Plasmodium vivax circumsporozoite protein; PvDBP, Plasmodium vivax Duffy-binding protein; Rh or RH, reticulocyte-binding protein homologue; SAPN, self-assembling protein nanoparticle; SSI, Statens Serum Institut (Denmark); U., University; UCAP, Université Cheikh Anta Diop (Senegal); UKT, Institute of Tropical Medicine, University of Tübingen (Germany); USAMMRC, US Army Medical Research and Materiel Command; WEHI, Walter and Eliza Hall Institute of Medical Research (Australia); WRAIR, Walter Reed Army Institute of Research (USA). *Sponsors of late-stage clinical trials. ‡Pending review or approval by WHO prequalification, or by regulatory bodies who are members or observers of the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH).
Management
No single drug is ideal against all Plasmodium spp. or all of the manifestations of the disease that occur in different patient populations. Thus, treatment must be tailored to each situation appropriately108,158. First, the treatment of uncomplicated malaria and that of severe malaria are distinct. In uncomplicated malaria, the treatment of choice is an oral medicine with high efficacy and a low adverse-effect profile. However, the preferred initial therapy in severe malaria requires rapid onset and includes the parenteral administration of an artemisinin derivative, which can rapidly clear the parasites from the blood, and it is also suitable for those patients who have changes in mental status (such as coma) that make swallowing oral medications impossible. For the treatment of malaria during pregnancy, the options are limited to the drugs that are known to be safe for both the expectant mother and the fetus, and different regimens are needed (Box 2). Different drugs are used for different Plasmodium spp., and the choice is usually driven more by drug resistance frequencies (which are lower in P. vivax, P. ovale, P. malariae and P. knowlesi than in P. falciparum) than by species differences as such. Thus, chloroquine, with its low cost and excellent safety, is used in most cases of non-P. falciparum malaria, where it remains effective, whereas P. falciparum malaria requires newer medicines that overcome resistance issues. The persistence of P. vivax and P. ovale hypnozoites, even after clearance of the stages that cause symptoms, necessitates additional treatments. Only primaquine targets hypnozoites.
P. falciparum malaria
The mainstay treatments for uncomplicated P. falciparum malaria are ACTs: fixed-dose combinations of two drugs, an artemisinin derivative and a quinine derivative108 (Box 4; Table 1).
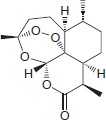
Owing to its high lipophilicity, artemisinin itself is not the molecule of choice in any stringent regulatory authority-approved combination. Instead, semisynthetic derivatives are used: namely, DHA (the reduced hemiacetal of the major active metabolite of many artemisinin derivatives), artesunate (a succinate prodrug of DHA that is highly water-soluble) or artemether (a methylether prodrug of DHA).
Quinine has been used in medicine for centuries159, but it was only in the mid-20th century that a synthetic form was made and the emerging pharmaceutical and government research sectors delivered the next-generation medicines that built on it. The combination partners of choice are 4-aminoquinolines (for example, amodiaquine, piperaquine and pyronaridine) and amino-alcohols (such as mefloquine or lumefantrine); these molecules are believed to interfere with haemozoin formation. There are now five ACTs that have been approved or are close to approval by the FDA, the European Medicines Agency (EMA) or WHO prequalification (Figs 7,8; Table 1). In pivotal clinical studies, these combinations have proven extremely effective (achieving an adequate clinical and parasitological response (that is, the absence of parasitaemia at day 28 in >94% of patients; for example, see Ref. 160), are well-tolerated (as they have been given to >300 million paediatric patients), are affordable (typically under US$1 per dose) and, thanks to ingenious formulations and packaging, are stable in tropical climate conditions.
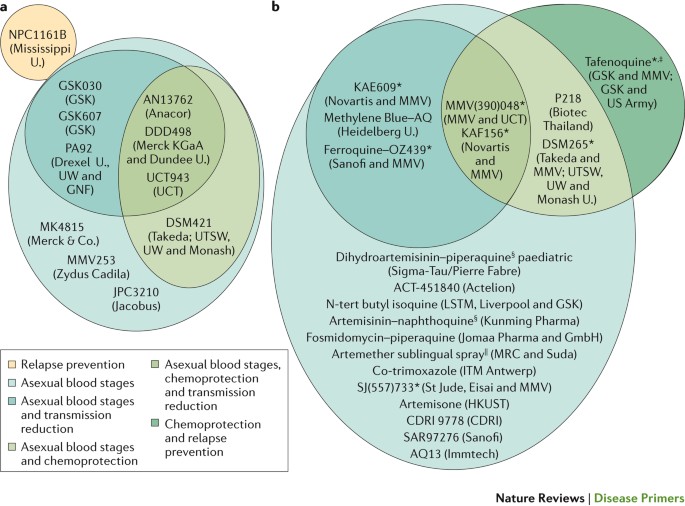
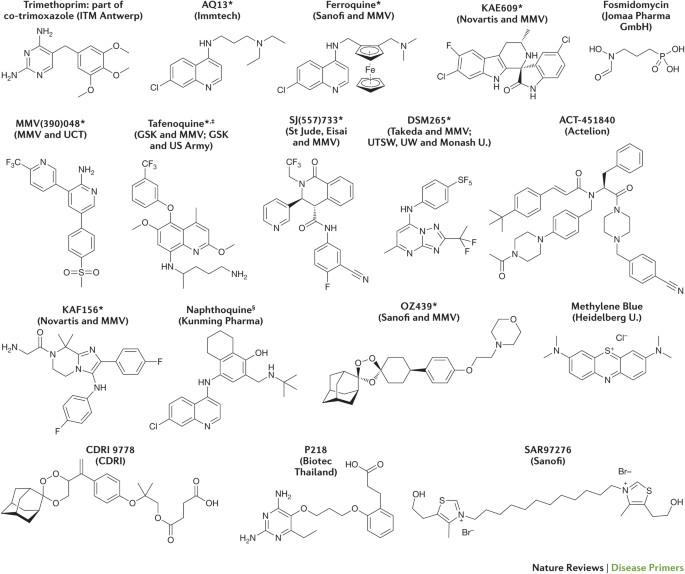
a | Preclinical candidates. b | Compounds or compound combinations that are in clinical development. The multitude of molecules that target only the asexual blood stages reflects the fact that many of these compounds are at an early stage of development, and further assessment of their Target Candidate Profile is still ongoing. KAF156 and KAE609 were discovered in a multiparty collaboration between the Novartis Institute for Tropical Disease (Singapore), the Genomics Institute of the Novartis Research Foundation (GNF; USA), the Swiss Tropical and Public Health Institute, the Biomedical Primate Research Centre (The Netherlands), the Wellcome Trust (UK) and Medicines for Malaria Venture (MMV). DSM265 was discovered through a collaboration involving the University of Texas Southwestern (UTSW; USA), the University of Washington (UW; USA), Monash University (Australia), GlaxoSmithKline (GSK) and MMV. MMV(390)048 was discovered through a collaboration involving the University of Cape Town (UCT; South Africa), the Swiss Tropical and Public Health Institute, Monash University, Syngene and MMV. SJ(557)733 was discovered in a collaboration involving St Jude Children's Research Hospital (USA), Rutgers University (USA), Monash University and MMV. Note that not all compounds are shown in this Figure, and updates can be found on the MMV website (www.mmv.org). CDRI, Central Drug Research Institute (India); ITM, Institute of Tropical Medicine; MRC, Medical Research Council; HKUST, Hong Kong University of Science and Technology; U., University. *Part of a combination that aims to be a new single-exposure radical cure (Target Product Profile 1). ‡Product that targets the prevention of relapse in Plasmodium vivax malaria. §3-day cure, artemisinin-based combination therapy. ||Severe malaria and pre-referral treatment.
See the Medicines for Malaria Venture (MMV) website (www.mmv.org) for updates. CDRI, Central Drug Research Institute (India); GSK, GlaxoSmithKline; ITM, Institute of Tropical Medicine; U., University; UCT, University of Cape Town (South Africa); UTSW, University of Texas Southwestern (USA); UW, University of Washington (USA). *Part of a combination that aims to be a new single-exposure radical cure (Target Product Profile 1). ‡Product that targets the prevention of relapse in Plasmodium vivax malaria. §3-day cure, artemisinin-based combination therapy.
Following the results of comprehensive studies in Africa and Asia, the injectable treatment of choice for severe P. falciparum malaria is artesunate161–163. In the United States, artesunate for intravenous use is available as an Investigational New Drug (IND) through the Centers for Disease Control and Prevention (CDC) malaria hotline and shows efficacies of >90% even in patients who are already unconscious161. Sometimes, however, in low-income countries, it is necessary to administer intravenous quinine or quinine while awaiting an artesunate supply. Suppositories of artesunate are in late-stage product development164 and are already available in Africa as a pre-referral treatment to keep patients alive while they reach a health clinic.
P. vivax malaria
Chloroquine or ACTs are WHO-recommended for uncomplicated P. vivax malaria108 (although chloroquine is no longer used in several countries, such as Indonesia). As chloroquine-resistant P. vivax is becoming increasingly widespread, particularly in Asia, the use of ACTs is increasing; although only artesunate–pyronaridine is approved for the treatment of blood-stage P. vivax malaria, the other ACTs are also effective and are used off-label. Relapses of P. vivax malaria present a problem in malaria control. Relapse frequencies differ among P. vivax strains; they are high (typically within 3 weeks) in all-year transmission areas, such as Papua New Guinea, but relapse occurs on average after 7 months in areas with a dry or winter season. Some P. vivax strains, such as the Moscow and North Korea strains, are not, in most cases, symptomatic at the time of first infection but become symptomatic only following reactivation of the hypnozoites165. Primaquine needs to be administered in addition to the primary treatment to prevent relapse and transmission, which can occur even years after the primary infection. Primaquine treatment, however, requires 14 days of treatment, has gastrointestinal adverse effects in some patients, and is contraindicated in pregnant women and in patients who are deficient in or express low levels of G6PD (as it can cause haemolysis). Tafenoquine166, a next-generation 8-aminoquinoline, is currently completing phase III clinical studies. As with patients receiving primaquine, patients receiving tafenoquine will still require an assessment of their G6PD enzyme activity to ensure safe use of the drug and to determine the optimal dose. In phase II studies, tafenoquine was shown to have an efficacy similar to that of primaquine but with a single dose only compared with the 7–14-day treatment with primaquine; higher patient compliance is expected to be a major benefit of a single-dose regimen. The ultimate elimination of P. vivax malaria will be dependent on the availability of safe and effective anti-relapse agents, and is, therefore, a major focus of the drug discovery community.
Drug resistance
The two drugs in ACTs have very different pharmacokinetic profiles in patients. The artemisinin components have a plasma half-life of only a few hours yet can reduce parasitaemia by three-to-four orders of magnitude. By contrast, the 4-aminoquinolines and amino-alcohols have long terminal half-lives (>4 days), providing cure (defined as an adequate clinical and parasitological response) and varying levels of post-treatment prophylaxis. The prolonged half-life of the non-artemisinin component of ACTs has raised concerns in the research community owing to the risk of drug resistance development. However, the effectiveness of the ACTs in rapidly reducing parasitaemia suggests that any emerging resistance has arisen largely as a result of poor clinical practice, including the use of artemisinin derivatives as monotherapy, a lack of patient compliance and substandard medicine quality (including counterfeits); these are all situations in which large numbers of parasites are exposed to a single active molecule167. However, resistance to piperaquine168 and partial resistance to artemisinin169 (which manifests as a reduced rate of parasite clearance rate rather than a shift in the half-maximal inhibitory concentration (IC50)) has been confirmed in the Greater Mekong subregion, as well as resistance to mefloquine and amodiaquine in various parts of the world170. Africa has so far been spared, but reports of treatment failure for either artemisinin171 or ACT172 in African isolates of P. falciparum have raised concerns. Thus, artemisinin-resistant Plasmodium spp. and insecticide-resistant mosquitoes are major threats to the progress that has been made in reducing the number of malaria-related deaths through current control programmes. It is important to emphasize that progress against malaria has historically been volatile; in many areas, the disease has re-emerged as the efficacy of old drugs has been lost in strains that developed resistance.
Many advances have been made in identifying genetic markers in Plasmodium spp. that correlate with resistance to clinically used drugs (Table 2). These markers enable the research and medical communities to proactively survey parasite populations to make informed treatment choices. Cross-resistance profiles reveal reciprocity between 4-aminoquinolines and amino-alcohols (that is, parasites resistant to one class are also less sensitive to the other). In addition, a drug can exert two opposite selective pressures: one towards the selection of resistant mutants and the other towards the selection of strains that have increased sensitivity to a different drug, a phenomenon known as ‘inverse selective pressure’ (Refs 173,174). These findings support the introduction of treatment rotation or triple combination therapies as potential future options. Finally, the drug discovery and development pipeline is delivering not only new compounds that have novel modes of action and overcome known resistant strains but also chemicals that have the potential to be effective in a single dose, which could overcome compliance issues. Nevertheless, policymakers need to be on high alert to prevent or rapidly eliminate outbreaks of resistant strains, and to prioritize the development of new treatments.
The drug discovery and development pipeline
The most comprehensive antimalarial discovery portfolio has been developed by the not-for-profit product development partnership Medicines for Malaria Venture (MMV) in collaboration with its partners in both academia and the pharmaceutical industry, with support from donors (mainly government agencies and philanthropic foundations) (Fig. 7). Promising compound series have been identified from three approaches: hypothesis-driven design to develop alternatives to marketed compounds (for example, synthetic peroxides such as ozonides); target-based screening and rational design (for example, screening of inhibitors of P. falciparum dihydroorotate dehydrogenase (PfDHODH)); and phenotypic screening175. Phenotypic screening has been the most successful approach to date, in terms of delivering preclinical candidates and identifying — through the sequencing of resistant mutants — novel molecular targets. However, with advances in the understanding of parasite biology and in molecular biology technology, target-based approaches will probably have a substantial role in coming years.
Two combinations — OZ439 (also known as artefenomel) with ferroquine (Sanofi and MMV) and KAF156 with lumefantrine (Novartis and MMV) — are about to begin phase IIb development to test the efficacy of single-dose cure and, in the case of KAF156–lumefantrine, also 2-day or 3-day cures. OZ439 is a fully synthetic peroxide for which sustained plasma exposure is achieved by a single oral dose in humans176,177; the hope is that it could replace the three independent doses required for artemisinin derivatives. Ferroquine is a next-generation 4-aminoquinoline without cross-resistance to chloroquine, amodiaquine or piperaquine178,179. KAF156 is a novel imidazolopiperazine that has an unknown mechanism of action180–182, but its resistance marker — P. falciparum cyclic amine resistance locus (pfcarl) — seems to encode a transporter on the endoplasmic reticulum membrane of the parasite. Interestingly, whereas OZ439 and ferroquine principally affect the asexual blood stages, KAF156 also targets both the asexual liver stage and the sexual gametocyte stage and, therefore, could have an effect on transmission.
Two other compounds, KAE609 (also known as cipargamin183,184) and DSM265 (Refs 185–188), are poised to begin phase IIb and are awaiting decisions on combination partners. KAE609 is a highly potent spiroindolone that provides parasite clearance in patients even more rapidly than peroxides; its assumed mode of action is the inhibition of PfATP4 (Fig. 3), which is encoded by its resistance marker and is a transporter on the parasite plasma membrane that regulates Na+ and H+ homeostasis. Inhibition of this channel, which was identified through the sequencing of resistant mutants, increases Na+ concentrations and pH, resulting in parasite swelling, rigidity and fragility, thereby contributing to host parasite clearance in the spleen in addition to intrinsic parasite killing. In addition, effects on cholesterol levels in the parasite plasma membrane have been noted that are also likely to contribute to parasite killing by leading to an increased rigidity that results in more rapid clearance in vivo189. DSM265 is a novel triazolopyrimidine that has both blood-stage and liver-stage activity, and that selectively inhibits PfDHODH (Fig. 3). It was optimized for drug-like qualities from a compound that was identified from a high-throughput screen of a small-molecule library186,190. DSM265 maintains a serum concentration that is above its minimum parasiticidal concentration in humans for 8 days, and has shown efficacy in both treatment and chemoprotection models in human volunteers in phase Ib trials185,188.
Within phase I, new compounds are first assessed for safety and pharmacokinetics, and then for efficacy against the asexual blood or liver stages of Plasmodium spp. using a controlled human malaria infection model in healthy volunteers144. This model provides a rapid and cost-effective early proof of principle and, by modelling the concentration–response correlation, increases the accuracy of dose predictions for further clinical studies. The 2-aminopyridine MMV(390)048 (also known as MMV048 (Refs 191,192)), SJ(557)733 (also known as (+)-SJ733 (Refs 57,193)) and P218 (Ref. 194) are currently progressing through phase I. MMV(390)048 inhibits PfPI(4)K (Fig. 3), and this inhibition affects the asexual liver and blood stages, as well as the sexual gametocyte stage. MMV(390)048 has good exposure in animal models192, suggesting that it could potentially be used in a single dose in combination with another drug. SJ(557)733, which is a dihydroisoquinoline, inhibits PfATP4 and is an alternative partner that has a completely different structure from that of KAE609, and it has excellent preclinical safety and development potential. P218 is currently being evaluated for testing in controlled human malaria infection cohorts.
A further eight compounds are undergoing active preclinical development195. Of these compounds, four are alternatives to the leading compounds that target established mechanisms: the aminopyrazole PA92 (also known as PA-21A092 (Ref. 196)) and the thiotriazole GSK030 (also known as GSK3212030A) both target PfATP4; DSM421 (Ref. 197) is a triazolopyrimidine alternative to DSM265; and UCT943 (also known as MMV642943)198 is an alternative to MMV(390)048. Three compounds show novel mechanisms of action or resistance markers: M5717 (also known as DDD498 or DDD107498 (Ref. 199)) inhibits P. falciparum elongation factor 2 (and, therefore, protein synthesis) and has outstanding efficacy against all parasite life-cycle stages; MMV253 (also known as AZ13721412)200 is a fast-acting triaminopyrimidine with a V-type ATPase as resistance marker; and AN13762 (also known as AN762) is a novel oxaborole201 with a novel resistance marker. All of these compounds have been developed through collaborations with MMV.
The eighth compound in active preclinical development, led by Jacobus Pharmaceuticals, is JPC3210 (Ref. 202), which is a novel aminocresol that improves upon the historical candidate (WR194965) that was developed by the Walter Reed Army Institute of Research and tested in patients at the time of the development of mefloquine in the 1970s. JPC3210 has an unknown mechanism of action and has potent, long-lasting efficacy in preclinical models, suggesting its potential to be used in a single dose for both treatment and prophylaxis202.
Quality of life
Malaria is one among the diseases of poverty. The WHO website states the following: “There is general agreement that poverty not only increases the risk of ill health and vulnerability of people, it also has serious implications for the delivery of effective health-care such as reduced demand for services, lack of continuity or compliance in medical treatment, and increased transmission of infectious diseases” (Ref. 203). The socioeconomic burden of malaria is enormous, and although the disease predominantly affects children, it is a serious obstacle to a country's development and economy204. Malaria is responsible for annual expenses of billions of euros in some African countries205. In many endemic areas, each individual suffers multiple episodes of malaria per year, with each episode causing a loss of school time for children and work time for their parents and guardians. Despite the declining trends in malaria morbidity and mortality, the figures are still disconcertingly high for a disease that is entirely preventable and treatable16.
Malaria also has long-term detrimental effects on the non-health-related quality of life of the affected population; it intensifies poverty by limiting education opportunities, as it leads to absenteeism in schools and reduced productivity at work16. The effects of acute illness normally drive families to seek urgent attention, which may consist of self-medication, if the disease is familiar to the household. Yet, even an episode of uncomplicated malaria can be potentially fatal, owing to a delay in promptly accessing efficacious antimalarial drugs. As malaria is so familiar to many households, patients — especially children — may be presented late for early diagnosis and treatment in health facilities. Late presentation prolongs morbidity, increases the risk of severe malaria, and deprives the families of income through direct expenses and reduced productivity. Frequent disease episodes experienced in the endemic areas as well as their possible complications can negatively affect child growth and nutrition, shortening the lives of children and family members. The neurological consequences can affect a child's ability to learn and become a self-reliant adult206–208, as they often occur during an important brain growth phase, when brain areas involved in higher learning (such as planning, decision-making, self-awareness and social sensitivity) mature. Cognitive deficits occurring during the early education years affect the entire family, as they impair the ability of the child to contribute to the well-being of the family as they grow and put additional strain on the parents, who may sometimes have to care for a substantially disabled child and, later, a disabled adult209.
Outlook
The agenda set by the WHO aims for malaria incidence and mortality to decrease by 90% over the next 15 years, with increasing numbers of countries that eliminate the disease210. Even if we achieve the ambitious goals set by the WHO, there will still be a child dying of malaria every 10 minutes in 2030. The ACTs are extraordinarily effective, and much of the disease burden could be reduced by the complete deployment and availability of these medicines. There are now two approved ACTs that are specifically designed (taste-masked and sweetened) for paediatric use.
However, the emergence of drug-resistant Plasmodium spp. and insecticide-resistant mosquitoes is a major concern. The first clinical reports of artemisinin resistance came from the Thai–Cambodian border region in the mid-2000s211. So far, resistant strains have not spread to Africa, and the severity of the malaria caused by artemisinin-resistant parasites is not different from that of disease caused by wild-type strains. However, if artemisinin derivatives became ineffective, no alternative first-line treatments would be available, as new therapies are still only in phase II clinical trials, and their safety and efficacy will need to be effectively assessed in the field before they can be deployed for widespread clinical use.
Diagnostics
Future diagnostics should address two main issues. First, new diagnostic tests would ideally be non-invasive and not require a blood sample. Many approaches have been piloted, including parasite antigen detection in saliva212 or urine213, the detection of specific volatile chemicals in breath214, and direct non-invasive measurements of iron-rich haemozoin in skin blood vessels215. Second, diagnostic tests should be able to detect drug-resistant strains directly in the point-of-care setting, rather than in sentinel sites, to provide better treatment and generate more-detailed epidemiological maps216. A next-generation amplicon-sequencing method suitable for use in endemic countries would enable the high-throughput detection of genetic mutations in six P. falciparum genes that are associated with resistance to antimalarial drugs, including ACTs, chloroquine and sulfadoxine–pyrimethamine217.
Malaria challenges
In addition to the length of the process of discovering and developing new drugs, insecticides and vaccines, in malaria there is the hurdle of the delivery of these new compounds, which first need to obtain approval from all local regulatory authorities. There is a trend for harmonization of the approval requirements among different authorities, with an initiative involving several regional African organizations, for example, to review data on behalf of many countries, similarly to the EMA reviewing files on behalf of all of the European Union countries. These events are paving the way to shorten the time from the end of clinical studies to the day of large-scale deployment, when affected populations will start to reap the benefits.
The move towards elimination and eradication
High-content cellular assays have become available to test inhibitors of transmission and compounds that target hypnozoites218,219. Discovery efforts for treatment and chemoprotection combinations conform to the malaria Target Product Profiles — a planning tool for therapeutic candidates that is based on FDA guidelines — to ensure that what is delivered has clinical relevance. The MMV has defined220 and updated221 Target Candidate Profiles (TCPs), which define the attributes that are required for the ideal medicines and have proven invaluable in guiding single-molecule optimization and decision-making.
The current focus is moving beyond TCP1 (which includes molecules that clear asexual blood-stage parasitaemia); the goal is to deliver compounds that do not simply treat patients and control symptoms but that also have biological activity that disrupts the life cycle of the parasite and hence break the transmission cycle, a step that is necessary in the move towards elimination. Particular areas of interest are anti-relapse agents for P. vivax malaria (TCP3; compounds that target hypnozoites), compounds that kill hepatic schizonts (TCP4) and protect against the onset of symptoms, and gametocytocidal compounds to block transmission (TCP5). Future projects include work on long-lasting endectocides (TCP6), such as ivermectin107. The MMV Discovery Portfolio also includes alternative compounds to the clinical frontrunners, molecules with new mechanisms of action (which target, for example, N-myristoyltransferase222, coenzyme A biosynthesis223, phenylalanyl tRNA synthetase224, prolyl225 tRNA synthetase, plasmepsin V226 and the Qi site of cytochrome bc1 (Ref. 227)) and compounds that seem to be resistance-proof (at least in vitro).
In conclusion, while much progress has been made towards reducing the burden of malaria, much work remains to be done if these gains are to bring lasting relief to those living under the threat of infection. Without a continued focus on developing new antimalarials and new approaches for diagnosis and vector control, malaria will continue to exert an unacceptable toll on people living in disease endemic areas.
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
How to cite this article
Phillips, M. A. et al. Malaria. Nat. Rev. Dis. Primers 3, 17050 (2017).
References
Miller, L. H., Ackerman, H. C., Su, X. Z. & Wellems, T. E. Malaria biology and disease pathogenesis: insights for new treatments. Nat. Med. 19, 156–167 (2013).
White, N. J. et al. Malaria. Lancet 383, 723–735 (2014).
Cowman, A. F., Healer, J., Marapana, D. & Marsh, K. Malaria: biology and disease. Cell 167, 610–624 (2016). References 1–3 comprehensively review malaria biology and the disease.
Baker, D. A. Malaria gametocytogenesis. Mol. Biochem. Parasitol. 172, 57–65 (2010).
Waters, A. P. Epigenetic roulette in blood stream Plasmodium: gambling on sex. PLoS Pathog. 12, e1005353 (2016).
White, N. J. Determinants of relapse periodicity in Plasmodium vivax malaria. Malar. J. 10, 297 (2011).
Wassmer, S. C. et al. Investigating the pathogenesis of severe malaria: a multidisciplinary and cross-geographical approach. Am. J. Trop. Med. Hyg. 93, 42–56 (2015). Comprehensively reviews the causes of severe malaria and ongoing research efforts to understand malaria pathophysiology.
Wassmer, S. C. & Grau, G. E. Severe malaria: what's new on the pathogenesis front? Int. J. Parasitol. 47, 145–152 (2017).
World Health Organization. Severe malaria. Trop. Med. Int. Health 19 (Suppl. 1), 7–131 (2014).
Dondorp, A. M. & Day, N. P. The treatment of severe malaria. Trans. R. Soc. Trop. Med. Hyg. 101, 633–634 (2007).
Bernabeu, M. & Smith, J. D. EPCR and malaria severity: the center of a perfect storm. Trends Parasitol. 33, 295–308 (2017). Reviews the molecular basis of parasite sequestration in the tissues, which leads to the obstruction of the microvasculature and severe disease, and discusses the key role of EPCR in these processes.
Bhatt, S. et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature 526, 207–211 (2015). Attempts to identify the relative contribution of different antimalaria measures in reducing the number of malaria cases over the 2000–2015 period.
Mitchell, S. N. et al. Mosquito biology. Evolution of sexual traits influencing vectorial capacity in anopheline mosquitoes. Science 347, 985–988 (2015).
Sinka, M. E. et al. The dominant Anopheles vectors of human malaria in Africa, Europe and the Middle East: occurrence data, distribution maps and bionomic precis. Parasit. Vectors 3, 117 (2010).
World Health Organization. Eliminating malaria: learning from the past, looking ahead. WHOhttp://www.path.org/publications/files/MCP_rbm_pi_rpt_8.pdf (2011).
World Health Organization. World malaria report 2015. WHOhttp://www.who.int/malaria/publications/world-malaria-report-2015/report/en/ (2015).
Florens, L. et al. A proteomic view of the Plasmodium falciparum life cycle. Nature 419, 520–526 (2002).
Gardner, M. J. et al. Genome sequence of the human malaria parasite Plasmodium falciparum. Nature 419, 498–511 (2002). Reports for the first time the P. falciparum genome, which has formed the basis for research into the molecular basis of pathogenesis and parasite biology; a modern-day understanding of the disease would not be possible without this groundbreaking work.
Winzeler, E. A. Advances in parasite genomics: from sequences to regulatory networks. PLoS Pathog. 5, e1000649 (2009).
Gething, P. W. et al. Mapping Plasmodium falciparum mortality in Africa between 1990 and 2015. N. Engl. J. Med. 375, 2435–2445 (2016).
Maitland, K. Severe malaria in African children — the need for continuing investment. N. Engl. J. Med. 375, 2416–2417 (2016).
Miller, L. H., Mason, S. J., Clyde, D. F. & McGinniss, M. H. The resistance factor to Plasmodium vivax in blacks. The Duffy-blood-group genotype, FyFy. N. Engl. J. Med. 295, 302–304 (1976). Describes the discovery that led to a molecular understanding of why most Africans are resistant to infection by P. vivax, thereby explaining the limited penetration of P. vivax in Africa.
Mercereau-Puijalon, O. & Menard, D. Plasmodium vivax and the Duffy antigen: a paradigm revisited. Transfus. Clin. Biol. 17, 176–183 (2010).
Howes, R. E. et al. Plasmodium vivax transmission in Africa. PLoS Negl. Trop. Dis. 9, e0004222 (2015).
Sutherland, C. J. et al. Two nonrecombining sympatric forms of the human malaria parasite Plasmodium ovale occur globally. J. Infect. Dis. 201, 1544–1550 (2010).
Cox-Singh, J. et al. Plasmodium knowlesi malaria in humans is widely distributed and potentially life threatening. Clin. Infect. Dis. 46, 165–171 (2008).
Singh, B. et al. A large focus of naturally acquired Plasmodium knowlesi infections in human beings. Lancet 363, 1017–1024 (2004). Describes the discovery that P. knowlesi, which was previously thought to primarily infect macaques, accounted for over half of the cases of malaria in their study in the Kapit district (Malaysia). Demonstrates for the first time that P. knowlesi should be considered as an emerging infectious disease in humans. Whether transmission via mosquitoes was occurring from monkey to man or from man to man remained an open question.
Brock, P. M. et al. Plasmodium knowlesi transmission: integrating quantitative approaches from epidemiology and ecology to understand malaria as a zoonosis. Parasitology 143, 389–400 (2016).
Imwong, M., Nakeesathit, S., Day, N. P. & White, N. J. A review of mixed malaria species infections in anopheline mosquitoes. Malar. J. 10, 253 (2011).
Ginouves, M. et al. Frequency and distribution of mixed Plasmodium falciparum–vivax infections in French Guiana between 2000 and 2008. Malar. J. 14, 446 (2015).
Srisutham, S. et al. Four human Plasmodium species quantification using droplet digital PCR. PLoS ONE 12, e0175771 (2017).
Armed Forces Health Surveillance Branch. Update: malaria, U. S. Armed Forces, 2016. MSMR 24, 2–7 (2017).
IISS: International Institute for Strategic Studies. Armed Conflict Survey 2016 (IISS, 2016).
Mueller, I. et al. Natural acquisition of immunity to Plasmodium vivax: epidemiological observations and potential targets. Adv. Parasitol. 81, 77–131 (2013).
Ataide, R., Mayor, A. & Rogerson, S. J. Malaria, primigravidae, and antibodies: knowledge gained and future perspectives. Trends Parasitol. 30, 85–94 (2014).
Desai, M. et al. Epidemiology and burden of malaria in pregnancy. Lancet Infect. Dis. 7, 93–104 (2007).
McGready, R. et al. Adverse effects of falciparum and vivax malaria and the safety of antimalarial treatment in early pregnancy: a population-based study. Lancet Infect. Dis. 12, 388–396 (2012).
Cohen, C. et al. Increased prevalence of severe malaria in HIV-infected adults in South Africa. Clin. Infect. Dis. 41, 1631–1637 (2005).
Mulu, A. et al. Epidemiological and clinical correlates of malaria–helminth co-infections in southern Ethiopia. Malar. J. 12, 227 (2013).
Gwamaka, M. et al. Iron deficiency protects against severe Plasmodium falciparum malaria and death in young children. Clin. Infect. Dis. 54, 1137–1144 (2012).
Neuberger, A., Okebe, J., Yahav, D. & Paul, M. Oral iron supplements for children in malaria-endemic areas. Cochrane Database Syst. Rev. 2, CD006589 (2016).
Tilley, L., Straimer, J., Gnadig, N. F., Ralph, S. A. & Fidock, D. A. Artemisinin action and resistance in Plasmodium falciparum . Trends Parasitol. 32, 682–696 (2016). Comprehensively reviews the emerging threat of artemisinin resistance, covering what is known about the mechanism of action of the drug and the molecular basis of artemisinin resistance.
Woodrow, C. J. & White, N. J. The clinical impact of artemisinin resistance in Southeast Asia and the potential for future spread. FEMS Microbiol. Rev. 41, 34–48 (2017).
Menard, D. et al. A worldwide map of Plasmodium falciparum K13-propeller polymorphisms. N. Engl. J. Med. 374, 2453–2464 (2016).
Imwong, M. et al. The spread of artemisinin-resistant Plasmodium falciparum in the greater Mekong subregion: a molecular epidemiology observational study. Lancet Infect. Dis. 17, 491–497 (2017).
Paul, A. S., Egan, E. S. & Duraisingh, M. T. Host–parasite interactions that guide red blood cell invasion by malaria parasites. Curr. Opin. Hematol. 22, 220–226 (2015). Reviews the molecular basis of parasite invasion.
Lim, C. et al. Reticulocyte preference and stage development of Plasmodium vivax isolates. J. Infect. Dis. 214, 1081–1084 (2016).
Boddey, J. A. & Cowman, A. F. Plasmodium nesting: remaking the erythrocyte from the inside out. Annu. Rev. Microbiol. 67, 243–269 (2013).
Spillman, N. J., Beck, J. R. & Goldberg, D. E. Protein export into malaria parasite-infected erythrocytes: mechanisms and functional consequences. Annu. Rev. Biochem. 84, 813–841 (2015). Reviews the biology associated with red blood cell remodelling upon parasite invasion.
Phillips, M. A. in Neglected Diseases and Drug Discovery (eds Palmer, M. & Wells, T. N. C. ) 65–87 (RCS Publishing, 2011).
Istvan, E. S. et al. Validation of isoleucine utilization targets in Plasmodium falciparum . Proc. Natl Acad. Sci. USA 108, 1627–1632 (2011).
Wunderlich, J., Rohrbach, P. & Dalton, J. P. The malaria digestive vacuole. Front. Biosci. (Schol. Ed.) 4, 1424–1448 (2012).
Chugh, M. et al. Protein complex directs hemoglobin-to-hemozoin formation in Plasmodium falciparum . Proc. Natl Acad. Sci. USA 110, 5392–5397 (2013).
Sigala, P. A. & Goldberg, D. E. The peculiarities and paradoxes of Plasmodium heme metabolism. Annu. Rev. Microbiol. 68, 259–278 (2014).
Spillman, N. J. et al. Na+ regulation in the malaria parasite Plasmodium falciparum involves the cation ATPase PfATP4 and is a target of the spiroindolone antimalarials. Cell Host Microbe 13, 227–237 (2013). Identifies the protein target of one of the key new antimalarials that is in clinical development.
Spillman, N. J. & Kirk, K. The malaria parasite cation ATPase PfATP4 and its role in the mechanism of action of a new arsenal of antimalarial drugs. Int. J. Parasitol. Drugs Drug Resist. 5, 149–162 (2015).
Jimenez-Diaz, M. B. et al. (+)-SJ733, a clinical candidate for malaria that acts through ATP4 to induce rapid host-mediated clearance of Plasmodium. Proc. Natl Acad. Sci. USA 111, E5455–E5462 (2014).
McNamara, C. W. et al. Targeting Plasmodium PI(4)K to eliminate malaria. Nature 504, 248–253 (2013). Identifies an important new target for drug discovery.
Rosenberg, R., Wirtz, R. A., Schneider, I. & Burge, R. An estimation of the number of malaria sporozoites ejected by a feeding mosquito. Trans. R. Soc. Trop. Med. Hyg. 84, 209–212 (1990).
Sinnis, P. & Zavala, F. The skin: where malaria infection and the host immune response begin. Semin. Immunopathol. 34, 787–792 (2012).
Frischknecht, F. et al. Imaging movement of malaria parasites during transmission by Anopheles mosquitoes. Cell. Microbiol. 6, 687–694 (2004).
Zheng, H., Tan, Z. & Xu, W. Immune evasion strategies of pre-erythrocytic malaria parasites. Mediators Inflamm. 2014, 362605 (2014).
Duraisingh, M. T. & Horn, D. Epigenetic regulation of virulence gene expression in parasitic protozoa. Cell Host Microbe 19, 629–640 (2016).
Smith, J. D. The role of PfEMP1 adhesion domain classification in Plasmodium falciparum pathogenesis research. Mol. Biochem. Parasitol. 195, 82–87 (2014).
Dobbs, K. R. & Dent, A. E. Plasmodium malaria and antimalarial antibodies in the first year of life. Parasitology 143, 129–138 (2016).
Fowkes, F. J., Boeuf, P. & Beeson, J. G. Immunity to malaria in an era of declining malaria transmission. Parasitology 143, 139–153 (2016).
Teo, A., Feng, G., Brown, G. V., Beeson, J. G. & Rogerson, S. J. Functional antibodies and protection against blood-stage malaria. Trends Parasitol. 32, 887–898 (2016).
Marsh, K. & Kinyanjui, S. Immune effector mechanisms in malaria. Parasite Immunol. 28, 51–60 (2006).
Parroche, P. et al. Malaria hemozoin is immunologically inert but radically enhances innate responses by presenting malaria DNA to Toll-like receptor 9. Proc. Natl Acad. Sci. USA 104, 1919–1924 (2007).
Karunaweera, N. D., Grau, G. E., Gamage, P., Carter, R. & Mendis, K. N. Dynamics of fever and serum levels of tumor necrosis factor are closely associated during clinical paroxysms in Plasmodium vivax malaria. Proc. Natl Acad. Sci. USA 89, 3200–3203 (1992).
Vijaykumar, M., Naik, R. S. & Gowda, D. C. Plasmodium falciparum glycosylphosphatidylinositol-induced TNF-α secretion by macrophages is mediated without membrane insertion or endocytosis. J. Biol. Chem. 276, 6909–6912 (2001).
Wijesekera, S. K., Carter, R., Rathnayaka, L. & Mendis, K. N. A malaria parasite toxin associated with Plasmodium vivax paroxysms. Clin. Exp. Immunol. 104, 221–227 (1996).
Hosseini, S. M. & Feng, J. J. How malaria parasites reduce the deformability of infected red blood cells. Biophys. J. 103, 1–10 (2012).
Gillrie M. R. et al. Thrombin cleavage of Plasmodium falciparum erythrocyte membrane protein 1 inhibits cytoadherence. mBio 7 e01120-16 (2016).
Bernabeu, M. et al. Severe adult malaria is associated with specific PfEMP1 adhesion types and high parasite biomass. Proc. Natl Acad. Sci. USA 113, E3270–E3279 (2016).
Fox, L. L. et al. Histidine-rich protein 2 plasma levels predict progression to cerebral malaria in Malawian children with Plasmodium falciparum infection. J. Infect. Dis. 208, 500–503 (2013).
Seydel, K. B. et al. Brain swelling and death in children with cerebral malaria. N. Engl. J. Med. 372, 1126–1137 (2015).
Lopez, C., Saravia, C., Gomez, A., Hoebeke, J. & Patarroyo, M. A. Mechanisms of genetically-based resistance to malaria. Gene 467, 1–12 (2010).
Piel, F. B. The present and future global burden of the inherited disorders of hemoglobin. Hematol. Oncol. Clin. North Am. 30, 327–341 (2016).
Elguero, E. et al. Malaria continues to select for sickle cell trait in Central Africa. Proc. Natl Acad. Sci. USA 112, 7051–7054 (2015).
Kwiatkowski, D. P. How malaria has affected the human genome and what human genetics can teach us about malaria. Am. J. Hum. Genet. 77, 171–192 (2005).
Cheng, Y. et al. Plasmodium vivax GPI-anchored micronemal antigen (PvGAMA) binds human erythrocytes independent of Duffy antigen status. Sci. Rep. 6, 35581 (2016).
Gunalan, K. et al. Role of Plasmodium vivax Duffy-binding protein 1 in invasion of Duffy-null Africans. Proc. Natl Acad. Sci. USA 113, 6271–6276 (2016).
Guindo, A., Fairhurst, R. M., Doumbo, O. K., Wellems, T. E. & Diallo, D. A. X-Linked G6PD deficiency protects hemizygous males but not heterozygous females against severe malaria. PLoS Med. 4, e66 (2007).
Cholera, R. et al. Impaired cytoadherence of Plasmodium falciparum-infected erythrocytes containing sickle hemoglobin. Proc. Natl Acad. Sci. USA 105, 991–996 (2008).
Fairhurst, R. M. et al. Abnormal display of PfEMP-1 on erythrocytes carrying haemoglobin C may protect against malaria. Nature 435, 1117–1121 (2005). References 84 and 86 identify key genetic traits that are associated with protection against P. falciparum malaria.
World Health Organization. Malaria: diagnostic testing. WHOhttp://www.who.int/malaria/areas/diagnosis/en/ (2016).
Worldwide Antimalarial Resistance Network (WWARN) AL Dose Impact Study Group. The effect of dose on the antimalarial efficacy of artemether–lumefantrine: a systematic review and pooled analysis of individual patient data. Lancet Infect. Dis. 15, 692–702 (2015). Describes data from the Worldwide Antimalarial Resistance Network (WWARN), which has set up computational tools that measure parasite reduction from human data; the WWARN also collects information on emerging resistance.
Joanny, F., Lohr, S. J., Engleitner, T., Lell, B. & Mordmuller, B. Limit of blank and limit of detection of Plasmodium falciparum thick blood smear microscopy in a routine setting in Central Africa. Malar. J. 13, 234 (2014).
Azikiwe, C. C. et al. A comparative laboratory diagnosis of malaria: microscopy versus rapid diagnostic test kits. Asian Pac. J. Trop. Biomed. 2, 307–310 (2012).
McCarthy, J. S. et al. A pilot randomised trial of induced blood-stage Plasmodium falciparum infections in healthy volunteers for testing efficacy of new antimalarial drugs. PLoS ONE 6, e21914 (2011). Describes the use of the human blood-stage challenge model for drug testing. This model has gone on to be an important tool for the early evaluation of the clinical efficacy of new antimalarial compounds.
Phiri, K. et al. Parasitological clearance rates and drug concentrations of a fixed dose combination of azithromycin–chloroquine in asymptomatic pregnant women with Plasmodium Falciparum parasitemia: an open-label, non-comparative study in sub-Saharan Africa. PLoS ONE 11, e0165692 (2016).
Imwong, M. et al. Numerical distributions of parasite densities during asymptomatic malaria. J. Infect. Dis. 213, 1322–1329 (2016).
Notomi, T. et al. Loop-mediated isothermal amplification of DNA. Nucleic Acids Res. 28, E63 (2000).
Sema, M. et al. Evaluation of non-instrumented nucleic acid amplification by loop-mediated isothermal amplification (NINA-LAMP) for the diagnosis of malaria in northwest Ethiopia. Malar. J. 14, 44 (2015).
Pholwat, S. et al. The malaria TaqMan array card includes 87 assays for Plasmodium falciparum drug resistance, identification of species, and genotyping in a single reaction. Antimicrob. Agents Chemother. 61 e00110-17 (2017).
Foundation for Innovative New Diagnostics. Acute febrile syndrome strategy. FiNDhttp://r4d.dfid.gov.uk/PDF/Outputs/FIND/0031-FIND-NMFI-document-print-inhouse.pdf (2012).
Gamboa, D. et al. A large proportion of P. falciparum isolates in the Amazon region of Peru lack pfhrp2 and pfhrp3: implications for malaria rapid diagnostic tests. PLoS ONE 5, e8091 (2010).
Akinyi, S. et al. Multiple genetic origins of histidine-rich protein 2 gene deletion in Plasmodium falciparum parasites from Peru. Sci. Rep. 3, 2797 (2013).
Cheng, Q. et al. Plasmodium falciparum parasites lacking histidine-rich protein 2 and 3: a review and recommendations for accurate reporting. Malar. J. 13, 283 (2014).
Bharti, P. K. et al. Prevalence of pfhrp2 and/or pfhrp3 gene deletion in Plasmodium falciparum population in eight highly endemic states in India. PLoS ONE 11, e0157949 (2016).
Deme, A. B. et al. Analysis of pfhrp2 genetic diversity in Senegal and implications for use of rapid diagnostic tests. Malar. J. 13, 34 (2014).
Parr, J. B. et al. Estimation of Plasmodium falciparum transmission intensity in Lilongwe, Malawi, by microscopy, rapid diagnostic testing, and nucleic acid detection. Am. J. Trop. Med. Hyg. 95, 373–377 (2016).
Mouatcho, J. C. & Goldring, J. P. Malaria rapid diagnostic tests: challenges and prospects. J. Med. Microbiol. 62, 1491–1505 (2013).
Soti, D. O. et al. Feasibility of an innovative electronic mobile system to assist health workers to collect accurate, complete and timely data in a malaria control programme in a remote setting in Kenya. Malar. J. 14, 430 (2015).
Scherr, T. F., Gupta, S., Wright, D. W. & Haselton, F. R. Mobile phone imaging and cloud-based analysis for standardized malaria detection and reporting. Sci. Rep. 6, 28645 (2016).
Ouédraogo, A. L. et al. Efficacy and safety of the mosquitocidal drug ivermectin to prevent malaria transmission after treatment: a double-blind, randomized, clinical trial. Clin. Infect. Dis. 60, 357–365 (2015).
World Health Organization. Guidelines for the treatment of malaria, 3rd edn. WHOhttp://apps.who.int/iris/bitstream/10665/162441/1/9789241549127_eng.pdf (2015).
Chanda, E., Remijo, C. D., Pasquale, H., Baba, S. P. & Lako, R. L. Scale-up of a programme for malaria vector control using long-lasting insecticide-treated nets: lessons from South Sudan. Bull. World Health Organ. 92, 290–296 (2014).
Ojuka, P. et al. Early biting and insecticide resistance in the malaria vector Anopheles might compromise the effectiveness of vector control intervention in southwestern Uganda. Malar. J. 14, 148 (2015).
Hemingway, J. et al. Averting a malaria disaster: will insecticide resistance derail malaria control? Lancet 387, 1785–1788 (2016). Discusses key issues relating to the continued control of the mosquito that transmits malaria.
Knapp, J., Macdonald, M., Malone, D., Hamon, N. & Richardson, J. H. Disruptive technology for vector control: the Innovative Vector Control Consortium and the US Military join forces to explore transformative insecticide application technology for mosquito control programmes. Malar. J. 14, 371 (2015).
Sibanda, M. & Focke, W. Development of an insecticide impregnated polymer wall lining for malaria vector control. Malar. J. 13 (Suppl. 1), 80 (2014).
Kruger, T., Sibanda, M. M., Focke, W. W., Bornman, M. S. & de Jager, C. Acceptability and effectiveness of a monofilament, polyethylene insecticide-treated wall lining for malaria control after six months in dwellings in Vhembe District, Limpopo Province, South Africa. Malar. J. 14, 485 (2015).
Burt, A. Heritable strategies for controlling insect vectors of disease. Phil. Trans. R. Soc. B 369, 20130432 (2014).
Committee on Gene Drive Research in Non-Human Organisms. Recommendations for Responsible Conduct. Gene Drives on the Horizon: Advancing Science, Navigating Uncertainty and Aligning Research with Public Values (National Academies Press, 2016).
Oliva, C. F. et al. Current status and future challenges for controlling malaria with the sterile insect technique: technical and social perspectives. Acta Trop. 132, S130–S139 (2014).
Bourtzis, K., Lees, R. S., Hendrichs, J. & Vreysen, M. J. More than one rabbit out of the hat: radiation, transgenic and symbiont-based approaches for sustainable management of mosquito and tsetse fly populations. Acta Trop. 157, 115–130 (2016).
Black, W. C. 4th, Alphey, L. & James, A. A. Why RIDL is not SIT. Trends Parasitol. 27, 362–370 (2011).
Windbichler, N. et al. A synthetic homing endonuclease-based gene drive system in the human malaria mosquito. Nature 473, 212–215 (2011).
Esvelt, K. M., Smidler, A. L., Catteruccia, F. & Church, G. M. Concerning RNA-guided gene drives for the alteration of wild populations. eLife 3, e03401 (2014).
Hammond, A. et al. A CRISPR–Cas9 gene drive system targeting female reproduction in the malaria mosquito vector Anopheles gambiae . Nat. Biotechnol. 34, 78–83 (2016).
Gantz, V. M. et al. Highly efficient Cas9-mediated gene drive for population modification of the malaria vector mosquito Anopheles stephensi . Proc. Natl Acad. Sci. USA 112, E6736–E6743 (2015).
Bull, J. J. & Turelli, M. Wolbachia versus dengue: evolutionary forecasts. Evol. Med. Public Health 2013, 197–207 (2013).
Wilke, A. B. & Marrelli, M. T. Paratransgenesis: a promising new strategy for mosquito vector control. Parasit. Vectors 8, 342 (2015).
Wang, S. et al. Fighting malaria with engineered symbiotic bacteria from vector mosquitoes. Proc. Natl Acad. Sci. USA 109, 12734–12739 (2012).
Lee, S. J., Ter Kuile, F. O., Price, R. N., Luxemburger, C. & Nosten, F. Adverse effects of mefloquine for the treatment of uncomplicated malaria in Thailand: a pooled analysis of 19, 850 individual patients. PLoS ONE 12, e0168780 (2017).
Spinner, C. D. et al. HIV pre-exposure prophylaxis (PrEP): a review of current knowledge of oral systemic HIV PrEP in humans. Infection 44, 151–158 (2016).
Margolis, D. A. & Boffito, M. Long-acting antiviral agents for HIV treatment. Curr. Opin. HIV AIDS 10, 246–252 (2015).
World Health Organization. WHO policy recommendation: seasonal malaria chemoprevention (SMC) for Plasmodium falciparum malaria control in highly seasonal transmission areas of the Sahel sub-region in Africa. WHOhttp://www.who.int/malaria/publications/atoz/who_smc_policy_recommendation/en/ (2012).
Cairns, M. et al. Estimating the potential public health impact of seasonal malaria chemoprevention in African children. Nat. Commun. 3, 881 (2012).
Noor, A. M. et al. Sub-national targeting of seasonal malaria chemoprevention in the Sahelian countries of the Nouakchott initiative. PLoS ONE 10, e0136919 (2015).
Tagbor, H. et al. Seasonal malaria chemoprevention in an area of extended seasonal transmission in Ashanti, Ghana: an individually randomised clinical trial. Trop. Med. Int. Health 21, 224–235 (2016).
Tine, R. C. et al. Feasibility, safety and effectiveness of combining home based malaria management and seasonal malaria chemoprevention in children less than 10 years in Senegal: a cluster-randomised trial. Trans. R. Soc. Trop. Med. Hyg. 108, 13–21 (2014).
Zongo, I. et al. Randomized noninferiority trial of dihydroartemisinin–piperaquine compared with sulfadoxine–pyrimethamine plus amodiaquine for seasonal malaria chemoprevention in Burkina Faso. Antimicrob. Agents Chemother. 59, 4387–4396 (2015).
Wilson, A. L. & IPTc Taskforce. A systematic review and meta-analysis of the efficacy and safety of intermittent preventive treatment of malaria in children (IPTc). PLoS ONE 6, e16976 (2011).
Matondo, S. I. et al. High levels of sulphadoxine–pyrimethamine resistance Pfdhfr–Pfdhps quintuple mutations: a cross sectional survey of six regions in Tanzania. Malar. J. 13, 152 (2014).
Gutman, J., Kovacs, S., Dorsey, G., Stergachis, A. & Ter Kuile, F. O. Safety, tolerability, and efficacy of repeated doses of dihydroartemisinin–piperaquine for prevention and treatment of malaria: a systematic review and meta-analysis. Lancet Infect. Dis. 17, 184–193 (2017).
Doolan, D. L., Dobano, C. & Baird, J. K. Acquired immunity to malaria. Clin. Microbiol. Rev. 22, 13–36 (2009).
Hoffman, S. L., Vekemans, J., Richie, T. L. & Duffy, P. E. The march toward malaria vaccines. Am. J. Prev. Med. 49, S319–S333 (2015).
Keegan, L. T. & Dushoff, J. Population-level effects of clinical immunity to malaria. BMC Infect. Dis. 13, 428 (2013).
McCarthy, J. S. et al. Experimentally induced blood-stage Plasmodium vivax infection in healthy volunteers. J. Infect. Dis. 208, 1688–1694 (2013).
Roestenberg, M. et al. Long-term protection against malaria after experimental sporozoite inoculation: an open-label follow-up study. Lancet 377, 1770–1776 (2011).
Engwerda, C. R., Minigo, G., Amante, F. H. & McCarthy, J. S. Experimentally induced blood stage malaria infection as a tool for clinical research. Trends Parasitol. 28, 515–521 (2012).
Wykes, M. N., Horne-Debets, J. M., Leow, C. Y. & Karunarathne, D. S. Malaria drives T cells to exhaustion. Front. Microbiol. 5, 249 (2014).
RTS,S Clinical Trials Partnership. Efficacy and safety of RTS,S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: final results of a phase 3, individually randomised, controlled trial. Lancet 386, 31–45 (2015). Describes a key clinical study that evaluates the efficacy of the only malaria vaccine that is currently at an advanced stage of clinical development.
Penny, M. A. et al. Public health impact and cost-effectiveness of the RTS,S/AS01 malaria vaccine: a systematic comparison of predictions from four mathematical models. Lancet 387, 367–375 (2015).
Gosling, R. & von Seidlein, L. The future of the RTS, S/AS01 malaria vaccine: an alternative development plan. PLoS Med. 13, e1001994 (2016). Describes strategies for effectively integrating the RTS,S/AS01 vaccine into malaria control strategies.
Hoffman, S. L. et al. Protection of humans against malaria by immunization with radiation-attenuated Plasmodium falciparum sporozoites. J. Infect. Dis. 185, 1155–1164 (2002).
Draper, S. J. et al. Recent advances in recombinant protein-based malaria vaccines. Vaccine 33, 7433–7443 (2015).
World Health Organization. WHO Product Development for Vaccines Advisory Committee (PD-VAC) meeting — 2015. WHOhttp://www.who.int/immunization/research/meetings_workshops/pdvac/en/ (2015).
Nunes, J. K. et al. Development of a transmission-blocking malaria vaccine: progress, challenges, and the path forward. Vaccine 32, 5531–5539 (2014).
Shimp, R. L. Jr et al. Development of a Pfs25–EPA malaria transmission blocking vaccine as a chemically conjugated nanoparticle. Vaccine 31, 2954–2962 (2013).
Kelley, B. Industrialization of mAb production technology: the bioprocessing industry at a crossroads. mAbs 1, 443–452 (2009).
Robbie, G. J. et al. A novel investigational Fc-modified humanized monoclonal antibody, motavizumab-YTE, has an extended half-life in healthy adults. Antimicrob. Agents Chemother. 57, 6147–6153 (2013).
US National Library of Medicine. ClinicalTrials.govhttps://clinicaltrials.gov/ct2/show/NCT01939899 (2017).
US National Library of Medicine. ClinicalTrials.govhttps://clinicaltrials.gov/ct2/show/NCT02647489 (2016).
Daily, J. P. Malaria 2017: update on the clinical literature and management. Curr. Infect. Dis. Rep.http://dx.doi.org/10.1007/s11908-017-0583-8 (2017).
Harrison, N. In celebration of the Jesuit's powder: a history of malaria treatment. Lancet Infect. Dis. 15, 1143 (2015).
Kinfu, G., Gebre-Selassie, S. & Fikrie, N. Therapeutic efficacy of artemether–lumefantrine for the treatment of uncomplicated Plasmodium falciparum malaria in northern Ethiopia. Malar. Res. Treat. 2012, 548710 (2012).
Sinclair, D., Donegan, S., Isba, R. & Lalloo, D. G. Artesunate versus quinine for treating severe malaria. Cochrane Database Syst. Rev. 6, CD005967 (2012).
Dondorp, A. et al. Artesunate versus quinine for treatment of severe falciparum malaria: a randomised trial. Lancet 366, 717–725 (2005). Describes a key study that demonstrates the efficacy of artesunate for the treatment of malaria and, therefore, supports the clinical use of artesunate.
Dondorp, A. M. et al. Artesunate versus quinine in the treatment of severe falciparum malaria in African children (AQUAMAT): an open-label, randomised trial. Lancet 376, 1647–1657 (2010).
Okebe, J. & Eisenhut, M. Pre-referral rectal artesunate for severe malaria. Cochrane Database Syst. Rev. 5, CD009964 (2014).
Verhave, J. P. Experimental, therapeutic and natural transmission of Plasmodium vivax tertian malaria: scientific and anecdotal data on the history of Dutch malaria studies. Parasit. Vectors 6, 19 (2013).
Llanos-Cuentas, A. et al. Tafenoquine plus chloroquine for the treatment and relapse prevention of Plasmodium vivax malaria (DETECTIVE): a multicentre, double-blind, randomised, phase 2b dose-selection study. Lancet 383, 1049–1058 (2014). Describes a key clinical study that demonstrates the efficacy of the only new compound that can prevent P. vivax relapse; tafenoquine and primaquine are the only compounds that have such activity.
White, N. J. Does antimalarial mass drug administration increase or decrease the risk of resistance? Lancet Infect. Dis. 17, e15–e20 (2017).
Amato, R. et al. Genetic markers associated with dihydroartemisinin–piperaquine failure in Plasmodium falciparum malaria in Cambodia: a genotype–phenotype association study. Lancet Infect. Dis. 17, 164–173 (2017).
Ariey, F. et al. A molecular marker of artemisinin-resistant Plasmodium falciparum malaria. Nature 505, 50–55 (2014).
World Health Organization. World malaria report 2016. WHOhttp://www.who.int/malaria/publications/world-malaria-report-2016/report/en/ (2016).
Lu, F. et al. Emergence of indigenous artemisinin-resistant Plasmodium falciparum in Africa. N. Engl. J. Med. 376, 991–993 (2017).
Sutherland, C. J. et al. Pfk13-independent treatment failure in four imported cases of Plasmodium falciparum malaria treated with artemether–lumefantrine in the United Kingdom. Antimicrob. Agents Chemother. 61 e02382-16 (2017).
Lukens, A. K. et al. Harnessing evolutionary fitness in Plasmodium falciparum for drug discovery and suppressing resistance. Proc. Natl Acad. Sci. USA 111, 799–804 (2014).
Taylor, A. R. et al. Artemether–lumefantrine and dihydroartemisinin–piperaquine exert inverse selective pressure on Plasmodium falciparum drug sensitivity-associated haplotypes in Uganda. Open Forum Infect. Dis. 4, ofw229 (2017).
Gamo, F. J. et al. Thousands of chemical starting points for antimalarial lead identification. Nature 465, 305–310 (2010).
Möhrle, J. J. et al. First-in-man safety and pharmacokinetics of synthetic ozonide OZ439 demonstrates an improved exposure profile relative to other peroxide antimalarials. Br. J. Clin. Pharmacol. 75, 524–537 (2013).
Phyo, A. P. et al. Antimalarial activity of artefenomel (OZ439), a novel synthetic antimalarial endoperoxide, in patients with Plasmodium falciparum and Plasmodium vivax malaria: an open-label phase 2 trial. Lancet Infect. Dis. 16, 61–69 (2016). Describes the key phase II clinical study of one of only two new clinical candidates that have reached phase IIb clinical development.
McCarthy, J. S. et al. A phase II pilot trial to evaluate safety and efficacy of ferroquine against early Plasmodium falciparum in an induced blood-stage malaria infection study. Malar. J. 15 469 (2016).
Held, J. et al. Ferroquine and artesunate in African adults and children with Plasmodium falciparum malaria: a phase 2, multicentre, randomised, double-blind, dose-ranging, non-inferiority study. Lancet Infect. Dis. 15, 1409–1419 (2015).
Leong, F. J. et al. A first-in-human randomized, double-blind, placebo-controlled, single- and multiple-ascending oral dose study of novel imidazolopiperazine KAF156 to assess its safety, tolerability, and pharmacokinetics in healthy adult volunteers. Antimicrob. Agents Chemother. 58, 6437–6443 (2014).
White, N. J. et al. Antimalarial activity of KAF156 in falciparum and vivax malaria. N. Engl. J. Med. 375, 1152–1160 (2016).
Kuhen, K. L. et al. KAF156 is an antimalarial clinical candidate with potential for use in prophylaxis, treatment and prevention of disease transmission. Antimicrob. Agents Chemother. 58, 5060–5067 (2014).
Huskey, S. E. et al. KAE609 (Cipargamin), a new spiroindolone agent for the treatment of malaria: evaluation of the absorption, distribution, metabolism, and excretion of a single oral 300- mg dose of [14C]KAE609 in healthy male subjects. Drug Metab. Dispos. 44, 672–682 (2016).
White, N. J. et al. Spiroindolone KAE609 for falciparum and vivax malaria. N. Engl. J. Med. 371, 403–410 (2014).
McCarthy, J. S. et al. Safety, tolerability, pharmacokinetics, and activity of the novel long-acting antimalarial DSM265: a two-part first-in-human phase 1a/1b randomised study. Lancet Infect. Dis. 17, 626–635 (2017). References 184 and 185 describe key clinical studies that support the efficacy of new antimalarials in the clinical development portfolio.
Phillips, M. A. et al. A long-duration dihydroorotate dehydrogenase inhibitor (DSM265) for prevention and treatment of malaria. Sci. Transl Med. 7, 296ra111 (2015). Describes the biological activity and product profile of the first inhibitor of PfDHODH to reach clinical development.
Rüeckle, T. et al. A phase IIa proof-of-concept study to assess the efficacy, safety, tolerability and pharmacokinetics of single doses of DSM265 in adult patients with acute, uncomplicated Plasmodium falciparum or vivax malaria mono-infection over a 28-day-extended observation period in Iquitos, Peru. ASTMHhttp://www.abstractsonline.com/Plan/ViewAbstract.aspx?sKey=2e5199c4-aceb-4d61-8769-342586917c5a&cKey=d7fda50e-36c6-4a28-a76b-96bad2ec308b&mKey=%7bAB652FDF-0111-45C7-A5E5-0BA9D4AF5E12%7d (2015).
Sulyok, M. et al. DSM265 for Plasmodium falciparum chemoprophylaxis: a randomised, double blinded, phase 1 trial with controlled human malaria infection. Lancet Infect. Dis. 17, 636–644 (2017). Describes the first use of a sporozoite human challenge study to demonstrate the chemopreventive activity of a compound that is under clinical development.
Das, S. et al. Na+ influx induced by new antimalarials causes rapid alterations in the cholesterol content and morphology of Plasmodium falciparum . PLoS Pathog. 12, e1005647 (2016).
Coteron, J. M. et al. Structure-guided lead optimization of triazolopyrimidine-ring substituents identifies potent Plasmodium falciparum dihydroorotate dehydrogenase inhibitors with clinical candidate potential. J. Med. Chem. 54, 5540–5561 (2011).
Ghidelli-Disse, S. et al. Identification of Plasmodium PI4 kinase as target of MMV390048 by chemoproteomics. Malar. J. 13, S21 (2014).
Paquet, T. et al. Antimalarial efficacy of MMV390048, an inhibitor of Plasmodium phosphatidylinositol 4-kinase. Sci. Transl Med. 9 eaad9735 (2017).
Ge, J. F. et al. Discovery of novel benzo[a]phenoxazine SSJ-183 as a drug candidate for malaria. ACS Med. Chem. Lett. 1, 360–364 (2010).
Abbat, S., Jain, V. & Bharatam, P. V. Origins of the specificity of inhibitor P218 toward wild-type and mutant PfDHFR: a molecular dynamics analysis. J. Biomol. Struct. Dyn. 33, 1913–1928 (2015).
Wells, T. N. C., Hooft van Huijsduijnen, R. & Van Voorhis, W. C. Malaria medicines: a glass half full? Nat. Rev. Drug Discov. 14, 424–442 (2015). Comprehensively reviews the malaria drug discovery pipeline.
Das, S. et al. Rapid reorganization of the parasite plasma membrane in response to a new class of antimalarial drugs. ISMMIDhttp://immid-is.drexelmed.edu/2014_ISMMID_Abstract.pdf (2014).
Phillips, M. A. et al. A triazolopyrimidine-based dihydroorotate dehydrogenase inhibitor with improved drug-like properties for treatment and prevention of malaria. ACS Infect. Dis. 2, 945–957 (2016).
Le Manach, C. et al. Identification of a potential antimalarial drug candidate from a series of 2-aminopyrazines by optimization of aqueous solubility and potency across the parasite life cycle. J. Med. Chem. 59, 9890–9905 (2016).
Baragaña, B. et al. A novel multiple-stage antimalarial agent that inhibits protein synthesis. Nature 522, 315–320 (2015).
Hameed, P. S. et al. Triaminopyrimidine is a fast-killing and long-acting antimalarial clinical candidate. Nat. Commun. 6, 6715 (2015).
Zhang, Y. K. et al. Synthesis and structure–activity relationships of novel benzoxaboroles as a new class of antimalarial agents. Bioorg. Med. Chem. Lett. 21, 644–651 (2011).
Chavchich, M. et al. Lead selection of the new aminomethylphenol, JPC-3210 for malaria treatment and prevention. Antimicrob. Agents Chemother. 60, 3115–3118 (2016).
Basch, P. Textbook of International Health 2nd edn (Oxford Univ. Press, 1999).
Ouattara, A. F. et al. Malaria knowledge and long-lasting insecticidal net use in rural communities of central Cote d’Ivoire. Malar. J. 10, 288 (2011).
Adetokunbo, O. & Gilles, H. Short Textbook of Public Health, Medicine for the Tropics (BookPower, 2006).
Carter, J. A. et al. Persistent neurocognitive impairments associated with severe falciparum malaria in Kenyan children. J. Neurol. Neurosurg. Psychiatry 76, 476–481 (2005).
Fernando, S. D., Rodrigo, C. & Rajapakse, S. The ‘hidden’ burden of malaria: cognitive impairment following infection. Malar. J. 9, 366 (2010).
Kihara, M., Carter, J. A. & Newton, C. R. The effect of Plasmodium falciparum on cognition: a systematic review. Trop. Med. Int. Health 11, 386–397 (2006).
Holding, P. A. & Snow, R. W. Impact of Plasmodium falciparum malaria on performance and learning: review of the evidence. Am. J. Trop. Med. Hyg. 64, 68–75 (2001).
World Health Organization. Global technical strategy for Malaria 2016–2030. WHOhttp://who.int/malaria/areas/global_technical_strategy/en/ (2016).
Noedl, H. et al. Evidence of artemisinin-resistant malaria in western Cambodia. N. Engl. J. Med. 359, 2619–2620 (2008).
Singh, R. et al. Comparison of three PCR-based assays for the non-invasive diagnosis of malaria: detection of Plasmodium parasites in blood and saliva. Eur. J. Clin. Microbiol. Infect. Dis. 33, 1631–1639 (2014).
Oguonu, T. et al. The performance evaluation of a urine malaria test (UMT) kit for the diagnosis of malaria in individuals with fever in South-east Nigeria: cross-sectional analytical study. Malar. J. 13, 403 (2014).
Berna, A. Z. et al. Analysis of breath specimens for biomarkers of Plasmodium falciparum infection. J. Infect. Dis. 212, 1120–1128 (2015).
Lukianova-Hleb, E. et al. Transdermal diagnosis of malaria using vapor nanobubbles. Emerg. Infect. Dis. 21, 1122–1127 (2015).
World Health Organization. Emergency response to artemisinin resistance in the greater Mekong subregion. Regional framework for action 2013–2015. WHOhttp://www.who.int/malaria/publications/atoz/9789241505321/en/ (2013).
Rao, P. N. et al. A method for amplicon deep sequencing of drug resistance genes in Plasmodium falciparum clinical isolates from India. J. Clin. Microbiol. 54, 1500–1511 (2016).
Wells, T. N., Burrows, J. N. & Baird, J. K. Targeting the hypnozoite reservoir of Plasmodium vivax: the hidden obstacle to malaria elimination. Trends Parasitol. 26, 145–151 (2010). Discusses issues related to targeting the latent stages of P. vivax to address the lack of drug options that are safe in all patients to treat these stages of the parasite.
Chattopadhyay, R. et al. Establishment of an in vitro assay for assessing the effects of drugs on the liver stages of Plasmodium vivax malaria. PLoS ONE 5, e14275 (2010).
Burrows, J. N., Hooft van Huijsduijnen, R., Möhrle, J. J., Oeuvray, C. & Wells, T. N. C. Designing the next generation of medicines for malaria control and eradication. Malar. J. 12, 187 (2013). Defines TCPs and Target Product Profiles for malaria.
Burrows, J. N. et al. New developments in anti-malarial target candidate and product profiles. Malar. J. 16, 26 (2017). Comprehensively analyses the compound properties that are required for the development of effective antimalarials that will cover all species and stages of the disease.
Tate, E. W., Bell, A. S., Rackham, M. D. & Wright, M. H. N-Myristoyltransferase as a potential drug target in malaria and leishmaniasis. Parasitology 141, 37–49 (2014).
Pett, H. E. et al. Novel pantothenate derivatives for anti-malarial chemotherapy. Malar. J. 14, 169 (2015).
Kato, N. et al. Diversity-oriented synthesis yields novel multistage antimalarial inhibitors. Nature 538, 344–349 (2016).
Herman, J. D. et al. The cytoplasmic prolyl-tRNA synthetase of the malaria parasite is a dual-stage target of febrifugine and its analogs. Sci. Transl Med. 7, 288ra277 (2015).
Russo, I. et al. Plasmepsin V licenses Plasmodium proteins for export into the host erythrocyte. Nature 463, 632–636 (2010).
Nilsen, A. et al. Quinolone-3-diarylethers: a new class of antimalarial drug. Sci. Transl Med. 5, 177ra137 (2013).
Newton, C. R., Taylor, T. E. & Whitten, R. O. Pathophysiology of fatal falciparum malaria in African children. Am. J. Trop. Med. Hyg. 58, 673–683 (1998).
Kalanon, M. & McFadden, G. I. Malaria. Plasmodium falciparum and its apicoplast. Biochem. Soc. Trans. 38, 775–782 (2010). Describes the importance of the apicoplast genome to the malaria parasite and opportunities to target this unique organelle for drug discovery.
Bozdech, Z. et al. The transcriptome of the intraerythrocytic developmental cycle of Plasmodium falciparum . PLoS Biol. 1, E5 (2003).
Hughes, K. R., Philip, N., Starnes, G. L., Taylor, S. & Waters, A. P. From cradle to grave: RNA biology in malaria parasites. Wiley Interdiscip. Rev. RNA 1, 287–303 (2010).
Llinas, M., Bozdech, Z., Wong, E. D., Adai, A. T. & DeRisi, J. L. Comparative whole genome transcriptome analysis of three Plasmodium falciparum strains. Nucleic Acids Res. 34, 1166–1173 (2006).
Ganesan, K. et al. A genetically hard-wired metabolic transcriptome in Plasmodium falciparum fails to mount protective responses to lethal antifolates. PLoS Pathog. 4, e1000214 (2008).
Hu, G. et al. Transcriptional profiling of growth perturbations of the human malaria parasite Plasmodium falciparum . Nat. Biotechnol. 28, 91–98 (2010).
Hoo, R. et al. Integrated analysis of the Plasmodium species transcriptome. EBioMedicine 7, 255–266 (2016).
Caro, F., Ahyong, V., Betegon, M. & DeRisi, J. L. Genome-wide regulatory dynamics of translation in the Plasmodium falciparum asexual blood stages. eLife 3, e04106 (2014). Describes a comprehensive analysis of the P. falciparum transcriptome over the red blood cell cycle.
Kirchner, S., Power, B. J. & Waters, A. P. Recent advances in malaria genomics and epigenomics. Genome Med. 8, 92 (2016). Comprehensively reviews of the role of epigenomics in gene expression in Plasmodium spp.
Lee, M. C. & Fidock, D. A. CRISPR-mediated genome editing of Plasmodium falciparum malaria parasites. Genome Med. 6, 63 (2014). Reviews genetic approaches to manipulating the P. falciparum genome.
de Koning-Ward, T. F., Gilson, P. R. & Crabb, B. S. Advances in molecular genetic systems in malaria. Nat. Rev. Microbiol. 13, 373–387 (2015). Reviews genetic approaches to manipulating the Plasmodium spp. genome.
Gomes, A. R. et al. A genome-scale vector resource enables high-throughput reverse genetic screening in a malaria parasite. Cell Host Microbe 17, 404–413 (2015).
Corey, V. C. et al. A broad analysis of resistance development in the malaria parasite. Nat. Commun. 7, 11901 (2016).
Allman, E. L., Painter, H. J., Samra, J., Carrasquilla, M. & Llinas, M. Metabolomic profiling of the malaria box reveals antimalarial target pathways. Antimicrob. Agents Chemother. 60, 6635–6649 (2016).
Manyando, C. et al. Safety of artemether–lumefantrine in pregnant women with malaria: results of a prospective cohort study in Zambia. Malar. J. 9, 249 (2010).
Yanow, S. K., Gavina, K., Gnidehou, S. & Maestre, A. Impact of malaria in pregnancy as Latin America approaches elimination. Trends Parasitol. 32, 416–427 (2016).
Harrington, W. E., Morrison, R., Fried, M. & Duffy, P. E. Intermittent preventive treatment in pregnant women is associated with increased risk of severe malaria in their offspring. PLoS ONE 8, e56183 (2013).
Dellicour, S. et al. First-trimester artemisinin derivatives and quinine treatments and the risk of adverse pregnancy outcomes in Africa and Asia: a meta-analysis of observational studies. PLoS Med. 14, e1002290 (2017).
Van Voorhis, W. C., Hooft van Huijsduijnen, R. & Wells, T. N. C. Profile of William C. Campbell, Satoshi O®mura, and Youyou Tu, 2015 Nobel Laureates in Physiology or Medicine. Proc. Natl Acad. Sci. USA 112, 15773–15776 (2015).
White, N. J., Hien, T. T. & Nosten, F. H. A. Brief history of qinghaosu. Trends Parasitol. 31, 607–610 (2015). Reviews the history of the discovery of artemisinin derivatives.
White, N. J. et al. Averting a malaria disaster. Lancet 353, 1965–1967 (1999).
White, N. J. & Olliaro, P. L. Strategies for the prevention of antimalarial drug resistance: rationale for combination chemotherapy for malaria. Parasitol. Today 12, 399–401 (1996).
Hien, T. T. & White, N. J. Qinghaosu. Lancet 341, 603–608 (1993).
Vaid, A., Ranjan, R., Smythe, W. A., Hoppe, H. C. & Sharma, P. PfPI3K, a phosphatidylinositol-3 kinase from Plasmodium falciparum, is exported to the host erythrocyte and is involved in hemoglobin trafficking. Blood 115, 2500–2507 (2010).
Mbengue, A. et al. A molecular mechanism of artemisinin resistance in Plasmodium falciparum malaria. Nature 520, 683–687 (2015).
Annan, Z. et al. Population genetic structure of Plasmodium falciparum in the two main African vectors. Anopheles gambiae and Anopheles funestus. Proc. Natl Acad. Sci. USA 104, 7987–7992 (2007).
Josling, G. A. & Llinas, M. Sexual development in Plasmodium parasites: knowing when it's time to commit. Nat. Rev. Microbiol. 13, 573–587 (2015).
Aly, A. S., Vaughan, A. M. & Kappe, S. H. Malaria parasite development in the mosquito and infection of the mammalian host. Annu. Rev. Microbiol. 63, 195–221 (2009).
World Health Organization. Climate change and human health. WHOhttp://www.who.int/globalchange/summary/en/index5.html (2017).
Gething, P. W. et al. Modelling the global constraints of temperature on transmission of Plasmodium falciparum and P. vivax. Parasit. Vectors 4, 92 (2011).
Weiss, G. E. et al. Revealing the sequence and resulting cellular morphology of receptor–ligand interactions during Plasmodium falciparum invasion of erythrocytes. PLoS Pathog. 11, e1004670 (2015).
Egan, E. S. et al. Malaria. A forward genetic screen identifies erythrocyte CD55 as essential for Plasmodium falciparum invasion. Science 348, 711–714 (2015).
Crosnier, C. et al. Basigin is a receptor essential for erythrocyte invasion by Plasmodium falciparum . Nature 480, 534–537 (2011). References 260 and 261 identify key receptors involved in P. falciparum invasion.
Volz, J. C. et al. Essential role of the PfRh5/PfRipr/CyRPA complex during Plasmodium falciparum invasion of erythrocytes. Cell Host Microbe 20, 60–71 (2016). Provides a comprehensive molecular understanding of the role of the receptor basigin in P. falciparum invasion and provides a comprehensive molecular model for the invasion process that highlights the three key steps.
Zenonos, Z. A. et al. Basigin is a druggable target for host-oriented antimalarial interventions. J. Exp. Med. 212, 1145–1151 (2015).
Srinivasan, P. et al. Binding of Plasmodium merozoite proteins RON2 and AMA1 triggers commitment to invasion. Proc. Natl Acad. Sci. USA 108, 13275–13280 (2011).
Remarque, E. J., Faber, B. W., Kocken, C. H. & Thomas, A. W. Apical membrane antigen 1: a malaria vaccine candidate in review. Trends Parasitol. 24, 74–84 (2008).
Yuthavong, Y. et al. Malarial dihydrofolate reductase as a paradigm for drug development against a resistance-compromised target. Proc. Natl Acad. Sci. USA 109, 16823–16828 (2012).
Sidhu, A. B., Verdier-Pinard, D. & Fidock, D. A. Chloroquine resistance in Plasmodium falciparum malaria parasites conferred by pfcrt mutations. Science 298, 210–213 (2002). Describes the identification of the molecular basis for chloroquine resistance.
Lek-Uthai, U. et al. Stronger activity of human immunodeficiency virus type 1 protease inhibitors against clinical isolates of Plasmodium vivax than against those of P. falciparum. Antimicrob. Agents Chemother. 52, 2435–2441 (2008).
World Health Organization. Rainbow tables. WHOhttp://www.who.int/immunization/research/development/Rainbow_tables/en/ (2017).
Mishra, N. et al. Emerging polymorphisms in falciparum Kelch 13 gene in northeastern region of India. Malar. J. 15, 583 (2016).
Spring, M. D. et al. Dihydroartemisinin–piperaquine failure associated with a triple mutant including kelch13 C580Y in Cambodia: an observational cohort study. Lancet Infect. Dis. 15, 683–691 (2015).
Thuy-Nhien, N. et al. K13-propeller mutations in Plasmodium falciparum populations in malaria endemic regions of Vietnam from 2009 to 2016. Antimicrob. Agents Chemother. 61, e01578-16 (2017).
Thanh, N. V. et al. Rapid decline in the susceptibility of Plasmodium falciparum to dihydroartemisinin–piperaquine in the south of Vietnam. Malar. J. 16, 27 (2017).
Sanchez, C. P. et al. Evidence for a pfcrt-associated chloroquine efflux system in the human malarial parasite Plasmodium falciparum . Biochemistry 44, 9862–9870 (2005).
Valderramos, S. G. & Fidock, D. A. Transporters involved in resistance to antimalarial drugs. Trends Pharmacol. Sci. 27, 594–601 (2006). Comprehensively reviews transporter mutants that are involved in resistance to the aminoquinoline series of antimalarial drugs (for example, chloroquine).
Borges, S. et al. Genomewide scan reveals amplification of mdr1 as a common denominator of resistance to mefloquine, lumefantrine, and artemisinin in Plasmodium chabaudi malaria parasites. Antimicrob. Agents Chemother. 55, 4858–4865 (2011).
Humphreys, G. S. et al. Amodiaquine and artemether–lumefantrine select distinct alleles of the Plasmodium falciparum mdr1 gene in Tanzanian children treated for uncomplicated malaria. Antimicrob. Agents Chemother. 51, 991–997 (2007).
Baliraine, F. N. & Rosenthal, P. J. Prolonged selection of pfmdr1 polymorphisms after treatment of falciparum malaria with artemether–lumefantrine in Uganda. J. Infect. Dis. 204, 1120–1124 (2011).
Martin, R. E. & Kirk, K. The malaria parasite's chloroquine resistance transporter is a member of the drug/metabolite transporter superfamily. Mol. Biol. Evol. 21, 1938–1949 (2004).
Ehrhardt, S. et al. Large-scale surveillance of Plasmodium falciparum crt(K76T) in northern Ghana. Antimicrob. Agents Chemother. 51, 3407–3409 (2007).
Figueiredo, P. et al. Prevalence of pfmdr1, pfcrt, pfdhfr and pfdhps mutations associated with drug resistance, in Luanda, Angola. Malar. J. 7, 236 (2008).
Mens, P. F. Ambiguous role of pfcrt K76 in Plasmodium falciparum: a marker of resistance or increased susceptibility. Expert Rev. Anti Infect. Ther. 7, 409–412 (2009).
Restrepo-Pineda, E., Arango, E., Maestre, A., Rosário, V. E. D. & Cravo, P. Studies on antimalarial drug susceptibility in Colombia, in relation to Pfmdr1 and Pfcrt. Parasitology 135, 547–553 (2008).
Drew, M. E. et al. Plasmodium food vacuole plasmepsins are activated by falcipains. J. Biol. Chem. 283, 12870–12876 (2008).
Witkowski, B. et al. A surrogate marker of piperaquine-resistant Plasmodium falciparum malaria: a phenotype–genotype association study. Lancet Infect. Dis. 17, 174–183 (2017).
Author information
Authors and Affiliations
Contributions
Introduction (M.A.P., J.N.B. and W.C.V.V.); Epidemiology (M.A.P. and W.C.V.V.); Mechanisms/pathophysiology (M.A.P.); Diagnosis, screening and prevention (M.A.P., J.N.B., R.H.v.H. and T.N.C.W.); Management (J.N.B., R.H.v.H. and T.N.C.W.); Quality of life (C.M.); Outlook (R.H.v.H. and T.N.C.W.); Overview of Primer (M.A.P.).
Corresponding author
Ethics declarations
Competing interests
T.N.C.W. is a non-executive director of Kymab in the United Kingdom. Kymab has programmes in malaria that are funded by the Bill & Melinda Gates Foundation. All other authors declare no competing interests.
Rights and permissions
About this article
Cite this article
Phillips, M., Burrows, J., Manyando, C. et al. Malaria. Nat Rev Dis Primers 3, 17050 (2017). https://doi.org/10.1038/nrdp.2017.50
Published:
DOI: https://doi.org/10.1038/nrdp.2017.50
This article is cited by
-
Gene expression analyses reveal differences in children’s response to malaria according to their age
Nature Communications (2024)
-
Histone modification analysis reveals common regulators of gene expression in liver and blood stage merozoites of Plasmodium parasites
Epigenetics & Chromatin (2023)
-
Impact of insecticide resistance on malaria vector competence: a literature review
Malaria Journal (2023)
-
High-throughput analysis of the transcriptional patterns of sexual genes in malaria
Parasites & Vectors (2023)
-
Development of a human malaria-on-a-chip disease model for drug efficacy and off-target toxicity evaluation
Scientific Reports (2023)